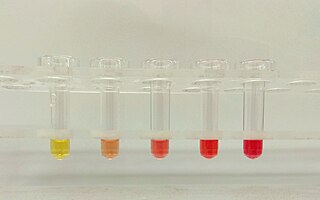
Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.
Serology is the scientific study of serum and other body fluids. In practice, the term usually refers to the diagnostic identification of antibodies in the serum. Such antibodies are typically formed in response to an infection, against other foreign proteins, or to one's own proteins. In either case, the procedure is simple.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.
The direct and indirect Coombs tests, also known as antiglobulin test (AGT), are blood tests used in immunohematology. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells they can cause anemia; this test can help clarify the condition. The indirect Coombs test detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells; the test can be carried out to diagnose reactions to a blood transfusion.
Warm antibody autoimmune hemolytic anemia (WAIHA) is the most common form of autoimmune haemolytic anemia. About half of the cases are of unknown cause, with the other half attributable to a predisposing condition or medications being taken. Contrary to cold autoimmune hemolytic anemia which happens in cold temperature (28–31 °C), WAIHA happens at body temperature.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5–10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Paroxysmal cold hemoglobinuria (PCH) or Donath–Landsteiner hemolytic anemia (DLHA) is an autoimmune hemolytic anemia featured by complement-mediated intravascular hemolysis after cold exposure. It can present as an acute non-recurrent postinfectious event in children, or chronic relapsing episodes in adults with hematological malignancies or tertiary syphilis. Described by Julius Donath (1870–1950) and Karl Landsteiner (1868–1943) in 1904, PCH is one of the first clinical entities recognized as an autoimmune disorder.
In ABO hemolytic disease of the newborn maternal IgG antibodies with specificity for the ABO blood group system pass through the placenta to the fetal circulation where they can cause hemolysis of fetal red blood cells which can lead to fetal anemia and HDN. In contrast to Rh disease, about half of the cases of ABO HDN occur in a firstborn baby and ABO HDN does not become more severe after further pregnancies.
Cold agglutinin disease (CAD) is a rare autoimmune disease characterized by the presence of high concentrations of circulating cold sensitive antibodies, usually IgM and autoantibodies that are also active at temperatures below 30 °C (86 °F), directed against red blood cells, causing them to agglutinate and undergo lysis. It is a form of autoimmune hemolytic anemia, specifically one in which antibodies bind red blood cells only at low body temperatures, typically 28–31 °C.
Hemolytic disease of the newborn (anti-Kell1) is the second most common cause of severe hemolytic disease of the newborn (HDN) after Rh disease. Anti-Kell1 is becoming relatively more important as prevention of Rh disease is also becoming more effective.
Hemolytic disease of the newborn (anti-Rhc) can range from a mild to a severe disease. It is the third most common cause of severe HDN. Rh disease is the most common and hemolytic disease of the newborn (anti-Kell) is the second most common cause of severe HDN. It occurs more commonly in women who are Rh D negative.
Hemolytic disease of the newborn (anti-RhE) is caused by the anti-RhE antibody of the Rh blood group system. The anti-RhE antibody can be naturally occurring, or arise following immune sensitization after a blood transfusion or pregnancy.
Acquired hemolytic anemia can be divided into immune and non-immune mediated forms of hemolytic anemia.
This page is currently under construction.

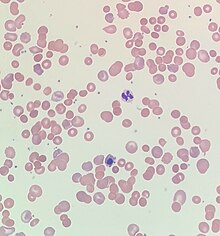
In hematology, red cell agglutination or autoagglutination is a phenomenon in which red blood cells clump together, forming aggregates. It is caused by the surface of the red cells being coated with antibodies. This often occurs in cold agglutinin disease, a type of autoimmune hemolytic anemia in which people produce antibodies that bind to their red blood cells at cold temperatures and destroy them. People may develop cold agglutinins from lymphoproliferative disorders, from infection with Mycoplasma pneumoniae or Epstein–Barr virus, or idiopathically. Red cell agglutination can also occur in paroxysmal nocturnal hemoglobinuria and warm autoimmune hemolytic anemia. In cases of red cell agglutination, the direct antiglobulin test can be used to demonstrate the presence of antibodies bound to the red cells.
Cold autoimmune hemolytic anemia caused by cold-reacting antibodies. Autoantibodies that bind to the erythrocyte membrane leading to premature erythrocyte destruction (hemolysis) characterize autoimmune hemolytic anemia.
Cold sensitive antibodies (CSA) are antibodies sensitive to cold temperature. Some cold sensitive antibodies are pathological and can lead to blood disorder. These pathological cold sensitive antibodies include cold agglutinins, Donath–Landsteiner antibodies, and cryoglobulins which are the culprits of cold agglutinin disease, paroxysmal cold hemoglobinuria in the process of Donath–Landsteiner hemolytic anemia, and vasculitis, respectively.
Mixed autoimmune hemolytic anemia (MAIHA) is a type of autoimmune hemolytic anemia which combines the features of cold sensitive antibody-induced diseases and warm autoimmune hemolytic anemia. The work-up for diagnosis is complex and the condition can be over-diagnosed.
Hemolytic jaundice, also known as prehepatic jaundice, is a type of jaundice arising from hemolysis or excessive destruction of red blood cells, when the byproduct bilirubin is not excreted by the hepatic cells quickly enough. Unless the patient is concurrently affected by hepatic dysfunctions or is experiencing hepatocellular damage, the liver does not contribute to this type of jaundice.