Ketamine is a dissociative anesthetic used medically for induction and maintenance of anesthesia. It is also used as a treatment for depression and pain management. It is a novel compound that was derived from phencyclidine in 1962 in pursuit of a safer anesthetic with fewer hallucinogenic effects.

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.

Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients. Depending on the procedure, general anaesthesia may be optional or required. Regardless of whether a patient may prefer to be unconscious or not, certain pain stimuli could result in involuntary responses from the patient that may make an operation extremely difficult. Thus, for many procedures, general anaesthesia is required from a practical perspective.

Propofol is the active component of an intravenous anesthetic formulation used for induction and maintenance of general anesthesia. It is chemically termed 2,6-diisopropylphenol. The formulation was approved under the brand name Diprivan. Numerous generic versions have since been released. Intravenous administration is used to induce unconsciousness after which anesthesia may be maintained using a combination of medications. It is manufactured as part of a sterile injectable emulsion formulation using soybean oil and lecithin, giving it a white milky coloration.

An anesthetic or anaesthetic is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two broad classes: general anesthetics, which result in a reversible loss of consciousness, and local anesthetics, which cause a reversible loss of sensation for a limited region of the body without necessarily affecting consciousness.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.
In immunology, systemic inflammatory response syndrome (SIRS) is an inflammatory state affecting the whole body. It is the body's response to an infectious or noninfectious insult. Although the definition of SIRS refers to it as an "inflammatory" response, it actually has pro- and anti-inflammatory components.
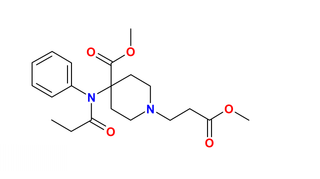
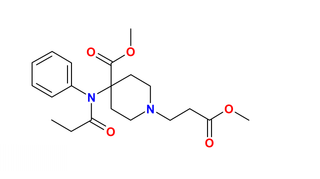
Remifentanil, marketed under the brand name Ultiva is a potent, short-acting synthetic opioid analgesic drug. It is given to patients during surgery to relieve pain and as an adjunct to an anaesthetic. Remifentanil is used for sedation as well as combined with other medications for use in general anesthesia. The use of remifentanil has made possible the use of high-dose opioid and low-dose hypnotic anesthesia, due to synergism between remifentanil and various hypnotic drugs and volatile anesthetics.
An induced coma – also known as a medically induced coma (MIC), barbiturate-induced coma, or drug-induced coma – is a temporary coma brought on by a controlled dose of an anesthetic drug, often a barbiturate such as pentobarbital or thiopental. Other intravenous anesthetic drugs such as midazolam or propofol may be used.
In anaesthesia and advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.
Distributive shock is a medical condition in which abnormal distribution of blood flow in the smallest blood vessels results in inadequate supply of blood to the body's tissues and organs. It is one of four categories of shock, a condition where there is not enough oxygen-carrying blood to meet the metabolic needs of the cells which make up the body's tissues and organs. Distributive shock is different from the other three categories of shock in that it occurs even though the output of the heart is at or above a normal level. The most common cause is sepsis leading to a type of distributive shock called septic shock, a condition that can be fatal.

The sequential organ failure assessment score, previously known as the sepsis-related organ failure assessment score, is used to track a person's status during the stay in an intensive care unit (ICU) to determine the extent of a person's organ function or rate of failure. The score is based on six different scores, one each for the respiratory, cardiovascular, hepatic, coagulation, renal and neurological systems.
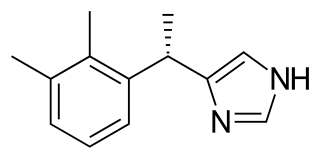
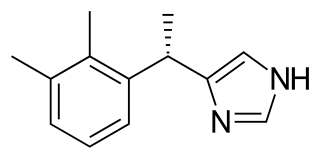
Dexmedetomidine, sold under the trade name Precedex among others, is a drug used in humans for sedation. Veterinarians use dexmedetomidine for similar purposes in treating cats, dogs, and horses. It is also used in humans to treat acute agitation associated with schizophrenia or bipolar I or II disorder.
Critical illness–related corticosteroid insufficiency is a form of adrenal insufficiency in critically ill patients who have blood corticosteroid levels which are inadequate for the severe stress response they experience. Combined with decreased glucocorticoid receptor sensitivity and tissue response to corticosteroids, this adrenal insufficiency constitutes a negative prognostic factor for intensive care patients.
Procedural sedation and analgesia (PSA) is a technique in which a sedating/dissociative medication is given, usually along with an analgesic medication, in order to perform non-surgical procedures on a patient. The overall goal is to induce a decreased level of consciousness while maintaining the patient's ability to breathe on their own. Airway protective reflexes are not compromised by this process and therefore endotracheal intubation is not required. PSA is commonly used in the emergency department, in addition to the operating room.

Propofol infusion syndrome (PRIS) is a rare syndrome which affects patients undergoing long-term treatment with high doses of the anaesthetic and sedative drug propofol. It can lead to cardiac failure, rhabdomyolysis, metabolic acidosis, and kidney failure, and is often fatal. High blood potassium, high blood triglycerides, and liver enlargement, proposed to be caused by either "a direct mitochondrial respiratory chain inhibition or impaired mitochondrial fatty acid metabolism" are also key features. It is associated with high doses and long-term use of propofol. It occurs more commonly in children, and critically ill patients receiving catecholamines and glucocorticoids are at high risk. Treatment is supportive. Early recognition of the syndrome and discontinuation of the propofol infusion reduces morbidity and mortality. Metabolic acidosis is a primary feature and may be the first laboratory evidence of the syndrome.

Coinduction in anesthesia is a pharmacological tool whereby a combination of sedative drugs may be used to greater effect than a single agent, achieving a smoother onset of general anesthesia. The use of coinduction allows lower doses of the same anesthetic agents to be used which provides enhanced safety, faster recovery, fewer side-effects, and more predictable pharmacodynamics. Coinduction is used in human medicine and veterinary medicine as standard practice to provide optimum anesthetic induction. The onset or induction phase of anesthesia is a critical period involving the loss of consciousness and reactivity in the patient, and is arguably the most dangerous period of a general anesthetic. A great variety of coinduction combinations are in use and selection is dependent on the patient's age and health, the specific situation, and the indication for anesthesia. As with all forms of anesthesia the resources available in the environment are a key factor.
Total intravenous anesthesia (TIVA) refers to the intravenous administration of anesthetic agents to induce a temporary loss of sensation or awareness. The first study of TIVA was done in 1872 using chloral hydrate, and the common anesthetic agent propofol was licensed in 1986. TIVA is currently employed in various procedures as an alternative technique of general anesthesia in order to improve post-operative recovery.

Ciprofol is a novel 2,6-disubstituted phenol derivative that is used for the intravenous induction of general anesthesia. A short-acting and highly selective γ-aminobutyric acid agonist, ciprofol is 4–6 times more potent than other phenol derivatives such as propofol or fospropofol.