General anaesthetics are often defined as compounds that induce a loss of consciousness in humans or loss of righting reflex in animals. Clinical definitions are also extended to include an induced coma that causes lack of awareness to painful stimuli, sufficient to facilitate surgical applications in clinical and veterinary practice. General anaesthetics do not act as analgesics and should also not be confused with sedatives. General anaesthetics are a structurally diverse group of compounds whose mechanisms encompass multiple biological targets involved in the control of neuronal pathways. The precise workings are the subject of some debate and ongoing research.

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

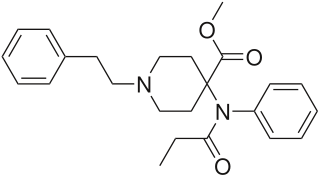
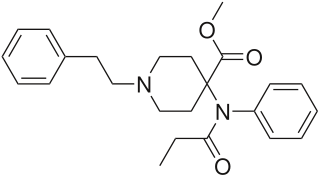
Fentanyl is a potent synthetic piperidine opioid primarily used as an analgesic. It is 50 times more potent than heroin and 100 times more potent than morphine; its primary clinical utility is in pain management for cancer patients and those recovering from painful surgeries. Fentanyl is also used as a sedative. Depending on the method of delivery, fentanyl can be very fast acting and ingesting a relatively small quantity can cause overdose. Fentanyl works by activating μ-opioid receptors. Fentanyl is sold under the brand names Actiq, Duragesic and Sublimaze, among others.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients. Depending on the procedure, general anaesthesia may be optional or required. Regardless of whether a patient may prefer to be unconscious or not, certain pain stimuli could result in involuntary responses from the patient that may make an operation extremely difficult. Thus, for many procedures, general anaesthesia is required from a practical perspective.

Propofol is the active component of an intravenous anesthetic formulation used for induction and maintenance of general anesthesia. It is chemically termed 2,6-diisopropylphenol. The formulation was approved under the brand name Diprivan. Numerous generic versions have since been released. Intravenous administration is used to induce unconsciousness after which anesthesia may be maintained using a combination of medications. It is manufactured as part of a sterile injectable emulsion formulation using soybean oil and lecithin, giving it a white milky coloration.

An anesthetic or anaesthetic is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two broad classes: general anesthetics, which result in a reversible loss of consciousness, and local anesthetics, which cause a reversible loss of sensation for a limited region of the body without necessarily affecting consciousness.
Carfentanil or carfentanyl, sold under the brand name Wildnil, is an extremely potent opioid analgesic used in veterinary medicine to anesthetize large animals such as elephants and rhinoceroses. It is typically administered in this context by tranquilizer dart. Carfentanil has also been used in humans to image opioid receptors. It has additionally been used as a recreational drug, typically by injection, insufflation, or inhalation. Deaths have been reported in association with carfentanil.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

Sufentanil, sold under the brand names Dsuvia and Sufenta, is a synthetic opioid analgesic drug approximately 5 to 10 times as potent as its parent drug, fentanyl, and 500 times as potent as morphine. Structurally, sufentanil differs from fentanyl through the addition of a methoxymethyl group on the piperidine ring, and the replacement of the phenyl ring by thiophene. Sufentanil first was synthesized at Janssen Pharmaceutica in 1974.

Nalbuphine, sold under the brand names Nubain among others, is an opioid analgesic which is used in the treatment of pain. It is given by injection into a vein, muscle, or fat.
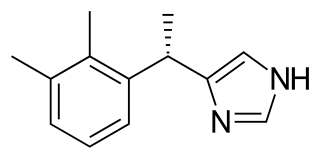
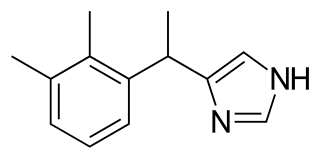
Dexmedetomidine, sold under the trade name Precedex among others, is a drug used in humans for sedation. Veterinarians use dexmedetomidine for similar purposes in treating cats, dogs, and horses. It is also used in humans to treat acute agitation associated with schizophrenia or bipolar I or II disorder.

Dihydroetorphine was developed by K. W. Bentley at McFarlan-Smith in the 1960s and is a potent opioid analgesic used mainly in China. It is a derivative of the better-known opioid etorphine, a very potent veterinary painkiller and anesthetic medication used primarily for the sedation of large animals such as elephants, giraffes, and rhinos.
Veterinary anesthesia is a specialization in the veterinary medicine field dedicated to the proper administration of anesthetic agents to non-human animals to control their consciousness during procedures. A veterinarian or a Registered Veterinary Technician administers these drugs to minimize stress, destructive behavior, and the threat of injury to both the patient and the doctor. The duration of the anesthesia process goes from the time before an animal leaves for the visit to the time after the animal reaches home after the visit, meaning it includes care from both the owner and the veterinary staff. Generally, anesthesia is used for a wider range of circumstances in animals than in people not only due to their inability to cooperate with certain diagnostic or therapeutic procedures, but also due to their species, breed, size, and corresponding anatomy. Veterinary anesthesia includes anesthesia of the major species: dogs, cats, horses, cattle, sheep, goats, and pigs, as well as all other animals requiring veterinary care such as birds, pocket pets, and wildlife.
Medetomidine is a synthetic drug used as both a surgical anesthetic and analgesic. It is often used as the hydrochloride salt, medetomidine hydrochloride, a crystalline white solid. It is an α2 adrenergic agonist that can be administered as an intravenous drug solution with sterile water.

Twilight anesthesia is an anesthetic technique where a mild dose of sedation is applied to induce anxiolysis, hypnosis, and anterograde amnesia. The patient is not unconscious, but sedated. During surgery or other medical procedures, the patient is under what is known as a "twilight state", where the patient is relaxed and "sleepy", able to follow simple directions by the doctor, and is responsive. Generally, twilight anesthesia causes the patient to forget the surgery and the time right after. It is used for a variety of surgical procedures and for various reasons. Just like regular anesthesia, twilight anesthesia is designed to help a patient feel more comfortable and to minimize pain associated with the procedure being performed and to allow the medical practitioner to practice without interruptions.

Patient-controlled analgesia (PCA) is any method of allowing a person in pain to administer their own pain relief. The infusion is programmable by the prescriber. If it is programmed and functioning as intended, the machine is unlikely to deliver an overdose of medication. Providers must always observe the first administration of any PCA medication which has not already been administered by the provider to respond to allergic reactions.

Coinduction in anesthesia is a pharmacological tool whereby a combination of sedative drugs may be used to greater effect than a single agent, achieving a smoother onset of general anesthesia. The use of coinduction allows lower doses of the same anesthetic agents to be used which provides enhanced safety, faster recovery, fewer side-effects, and more predictable pharmacodynamics. Coinduction is used in human medicine and veterinary medicine as standard practice to provide optimum anesthetic induction. The onset or induction phase of anesthesia is a critical period involving the loss of consciousness and reactivity in the patient, and is arguably the most dangerous period of a general anesthetic. A great variety of coinduction combinations are in use and selection is dependent on the patient's age and health, the specific situation, and the indication for anesthesia. As with all forms of anesthesia the resources available in the environment are a key factor.
Total intravenous anesthesia (TIVA) refers to the intravenous administration of anesthetic agents to induce a temporary loss of sensation or awareness. The first study of TIVA was done in 1872 using chloral hydrate, and the common anesthetic agent propofol was licensed in 1986. TIVA is currently employed in various procedures as an alternative technique of general anesthesia in order to improve post-operative recovery.

Remifentanilic acid is a metabolite of the potent short-acting synthetic opioid analgesic drug remifentanil. It is an analog of fentanyl and remifentanil, but is not active as an opioid in its own right.

Talmage D. Egan is an anesthesiologist, academic, entrepreneur, and author. He is a professor and chair in the department of anesthesiology, and an adjunct professor in the departments of pharmaceutics, bioengineering, and neurosurgery at the University of Utah School of Medicine.