Heroin, also known as diacetylmorphine and diamorphine among other names, is a morphinan opioid substance synthesized from the dried latex of the Papaver somniferum plant; it is mainly used as a recreational drug for its euphoric effects. Medical-grade diamorphine is used as a pure hydrochloride salt. Various white and brown powders sold illegally around the world as heroin are routinely diluted with cutting agents. Black tar heroin is a variable admixture of morphine derivatives—predominantly 6-MAM (6-monoacetylmorphine), which is the result of crude acetylation during clandestine production of street heroin. Heroin is used medically in several countries to relieve pain, such as during childbirth or a heart attack, as well as in opioid replacement therapy.
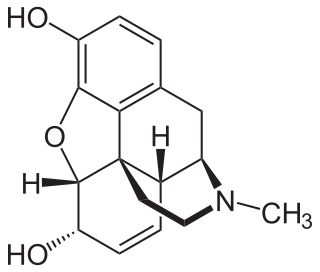
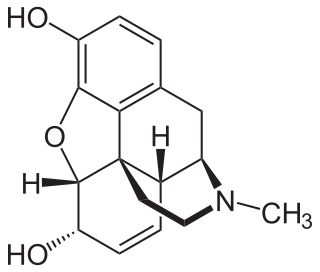
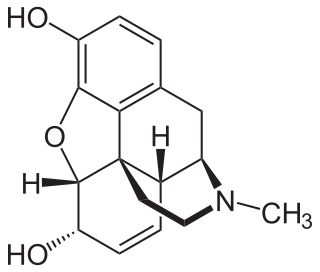
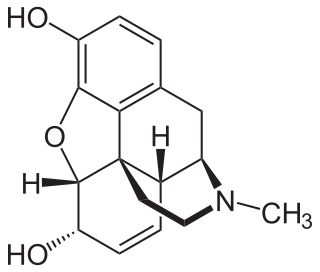
Morphine, formerly also called morphia, is a strong opiate that is found naturally in opium, a dark brown resin produced by drying the latex of opium poppies. It is mainly used as an analgesic. There are numerous methods used to administer morphine: oral; sublingual; via inhalation; injection into a muscle, injection under the skin, or injection into the spinal cord area; transdermal; or via rectal suppository. It acts directly on the central nervous system (CNS) to induce analgesia and alter perception and emotional response to pain. Physical and psychological dependence and tolerance may develop with repeated administration. It can be taken for both acute pain and chronic pain and is frequently used for pain from myocardial infarction, kidney stones, and during labor. Its maximum effect is reached after about 20 minutes when administered intravenously and 60 minutes when administered by mouth, while the duration of its effect is 3–7 hours. Long-acting formulations of morphine are available as MS-Contin, Kadian, and other brand names as well as generically.
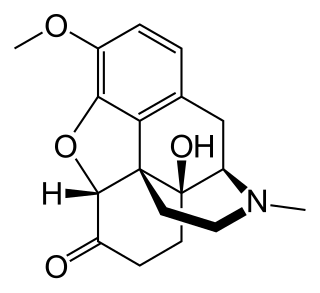
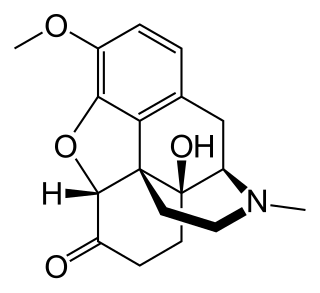
Oxycodone, sold under various brand names such as Roxicodone and OxyContin, is a semi-synthetic opioid used medically for treatment of moderate to severe pain. It is highly addictive and is a commonly abused drug. It is usually taken by mouth, and is available in immediate-release and controlled-release formulations. Onset of pain relief typically begins within fifteen minutes and lasts for up to six hours with the immediate-release formulation. In the United Kingdom, it is available by injection. Combination products are also available with paracetamol (acetaminophen), ibuprofen, naloxone, naltrexone, and aspirin.

Naloxone is an opioid antagonist: a medication used to reverse or reduce the effects of opioids. For example, it is used to restore breathing after an opioid overdose. Effects begin within two minutes when given intravenously, five minutes when injected into a muscle, and ten minutes as a nasal spray. Naloxone blocks the effects of opioids for 30 to 90 minutes.

Hydromorphone, also known as dihydromorphinone, and sold under the brand name Dilaudid among others, is a morphinan opioid used to treat moderate to severe pain. Typically, long-term use is only recommended for pain due to cancer. It may be used by mouth or by injection into a vein, muscle, or under the skin. Effects generally begin within half an hour and last for up to five hours. A 2016 Cochrane review found little difference in benefit between hydromorphone and other opioids for cancer pain.
Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. As a class of substances, they act on opioid receptors to produce morphine-like effects.
Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, the patient must have moderate opioid withdrawal symptoms before buprenorphine can be administered under direct observation of a health-care provider.

Naltrexone, sold under the brand name Revia among others, is a medication primarily used to manage alcohol use or opioid use disorder by reducing cravings and feelings of euphoria associated with substance use disorder. It has also been found effective in the treatment of other addictions and may be used for them off-label. An opioid-dependent person should not receive naltrexone before detoxification. It is taken by mouth or by injection into a muscle. Effects begin within 30 minutes, though a decreased desire for opioids may take a few weeks to occur. Side effects may include trouble sleeping, anxiety, nausea, and headaches. In those still on opioids, opioid withdrawal may occur. Use is not recommended in people with liver failure. It is unclear if use is safe during pregnancy. Naltrexone is an opioid antagonist and works by blocking the effects of opioids, including both opioid drugs as well as opioids naturally produced in the brain.

An opioid antagonist, or opioid receptor antagonist, is a receptor antagonist that acts on one or more of the opioid receptors.
Opioid-induced hyperalgesia (OIH) or opioid-induced abnormal pain sensitivity, also called paradoxical hyperalgesia, is an uncommon condition of generalized pain caused by the long-term use of high dosages of opioids such as morphine, oxycodone, and methadone. OIH is not necessarily confined to the original affected site. This means that if the person was originally taking opioids due to lower back pain, when OIH appears, the person may experience pain in the entire body, instead of just in the lower back. Over time, individuals taking opioids can also develop an increasing sensitivity to noxious stimuli, even evolving a painful response to previously non-noxious stimuli (allodynia). This means that if the person originally felt pain from twisting or from sitting too long, the person might now additionally experience pain from a light touch or from raindrops falling on the skin.
Drug detoxification is variously construed or interpreted as a type of "medical" intervention or technique in regards to a physical dependence mediated by a drug; as well as the process and experience of a withdrawal syndrome or any of the treatments for acute drug overdose (toxidrome). The first definition however, in relation to substance dependence and its treatment is arguably a misnomer and even directly contradictory since withdrawal is neither contingent upon nor alleviated through biological excretion or clearance of the drug. In fact, excretion of a given drug from the body is one of the very processes that leads to withdrawal since the syndrome arises largely due to the cessation itself and the drug being absent from the body; especially the blood plasma, not from ‘leftover toxins’ or traces of the drug still being in the system.

RB-101 is a drug that acts as an enkephalinase inhibitor, which is used in scientific research.
An equianalgesic chart is a conversion chart that lists equivalent doses of analgesics. Equianalgesic charts are used for calculation of an equivalent dose between different analgesics. Tables of this general type are also available for NSAIDs, benzodiazepines, depressants, stimulants, anticholinergics and others.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia from slow and shallow breathing. Other symptoms include small pupils and unconsciousness; however, its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.

An opiate is an alkaloid substance derived from opium. It differs from the similar term opioid in that the latter is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain. Opiates are alkaloid compounds naturally found in the opium poppy plant Papaver somniferum. The psychoactive compounds found in the opium plant include morphine, codeine, and thebaine. Opiates have long been used for a variety of medical conditions, with evidence of opiate trade and use for pain relief as early as the eighth century AD. Most opiates are considered drugs with moderate to high abuse potential and are listed on various "Substance-Control Schedules" under the Uniform Controlled Substances Act of the United States of America.

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek.

Harris Isbell was an American pharmacologist and the director of research for the NIMH Addiction Research Center at the Public Health Service Hospital in Lexington, Kentucky from 1945 to 1963. He did extensive research on the physical and psychological effects of various drugs on humans. Early work investigated aspects of physical dependence with opiates and barbiturates, while later work investigated psychedelic drugs, including LSD. The research was extensively reported in academic journals such as the Journal of Pharmacology and Experimental Therapeutics, Psychopharmacologia, and the AMA Archives of Neurology and Psychiatry.
Clinical Opiate Withdrawal Scale (COWS) is a method used by registered practitioners to measure the severity of a patient's opioid withdrawal symptoms. This method consists of a series of 11 topics each comprising 4 - 5 common symptoms experienced by a patient undergoing opioid withdrawal. In each topic a rank is given depending on what the patient responds to. Generally, 0 is considered to be no symptom shown and 4 or 5 is considered to be the most common and severe symptom shown. These results are then added up and a final diagnosis is made based on the value obtained. This test is crucial as it allows the practitioner to assess the physiological and psychological behaviours of the patient as well as the severity of each symptom during the duration of the examination. The results are grouped into 3 categories of mild, moderately severe and severe. Mild consists of 5 to 12 points, moderately severe consists of 13 to 24 points and anything above 36 points is severe and requires direct medical attention.
Opioid agonist therapy (OAT) is a treatment in which prescribed opioid agonists are given to patients who live with Opioid use disorder (OUD). In the case of methadone maintenance treatment (MMT), methadone is used to treat dependence on heroin or other opioids, and is administered on an ongoing basis.