Algeria is the largest country in Africa and is estimated to have a population of around 40 million people. Algeria has a public health care system, which is accessible and free of charge to all citizens of Algeria. The public health care system is financed by the government of Algeria. Given Algeria's young population, policy favors preventive health care and clinics over hospitals. In keeping with this policy, the government maintains an intensive immunization programme and a policy which allows Algerian citizens health care for Hospitalisations, medicines and outpatient care free to all citizens of Algeria.
In terms of available healthcare and health status Sierra Leone is rated very poorly. Globally, infant and maternal mortality rates remain among the highest. The major causes of illness within the country are preventable with modern technology and medical advances. Most deaths within the country are attributed to nutritional deficiencies, lack of access to clean water, pneumonia, diarrheal diseases, anemia, malaria, tuberculosis and HIV/AIDS.
Health in the Comoros continues to face public health problems characteristic of developing countries. After Comoros's independence in 1975, the French withdrew their medical teams, leaving the three islands' already rudimentary health care system in a state of severe crisis. French assistance was eventually resumed, and other nations also contributed medical assistance to the young republic.
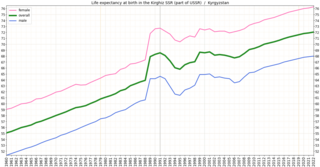
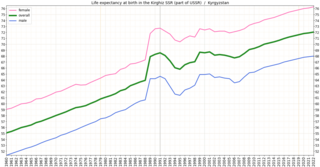
In the post-Soviet era, Kyrgyzstan's health system has suffered increasing shortages of health professionals and medicine. Kyrgyzstan must import nearly all its pharmaceuticals. The increasing role of private health services has supplemented the deteriorating state-supported system. In the early 2000s, public expenditures on health care decreased as a percentage of total expenditures, and the ratio of population to number of doctors increased substantially, from 296 per doctor in 1996 to 355 per doctor in 2001. A national primary-care health system, the Manas Program, was adopted in 1996 to restructure the Soviet system that Kyrgyzstan inherited. The number of people participating in this program has expanded gradually, and province-level family medicine training centers now retrain medical personnel. A mandatory medical insurance fund was established in 1997.

In terms of major health indicators, health in Paraguay ranks near the median among South American countries. In 2003 Paraguay had a child mortality rate of 29.5 deaths per 1,000 children, ranking it behind Argentina, Colombia, and Uruguay but ahead of Brazil and Bolivia. The health of Paraguayans living outside urban areas is generally worse than those residing in cities. Many preventable diseases, such as Chagas' disease, run rampant in rural regions. Parasitic and respiratory diseases, which could be controlled with proper medical treatment, drag down Paraguay's overall health. In general, malnutrition, lack of proper health care, and poor sanitation are the root of many health problems in Paraguay.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).
The Human Rights Measurement Initiative finds that Equatorial Guinea is fulfilling 43.5% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Equatorial Guinea achieves 64.4% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 58.8% of what is expected based on the nation's level of income. Equatorial Guinea falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 7.3% of what the nation is expected to achieve based on the resources (income) it has available.
The Republic of Moldova has a universal health care system.
Mauritius had a life expectancy of 75.17 years in 2014. 39% of Mauritian men smoked in 2014. 13% of men and 23% of women were obese in 2008.
The Republic of the Congo faces a number of ongoing health challenges.
For the period between 2005 and 2010, El Salvador had the third-lowest birth rate in Central America, with 22.8 births per 1,000. However, during the same period, it had the highest death rate in Central America, 5.9 deaths per 1,000. In 2015 life expectancy for men were 67.8 years and 77.0 years for women. Healthy life expectancy was 57 for males and 62 for females in 2003. There was considerable improvement in socioeconomic and health status from 1990 to 2015. On June 22, 2020, the Hospital El Salvador, a permanent hospital conversion of the convention center in San Salvador, was opened to the public; it is Latin America's largest hospital and was built to receive COVID-19 patients.
The fertility rate was approximately 3.7 per woman in Honduras in 2009. The under-five mortality rate is at 40 per 1,000 live births. The health expenditure was US$197 per person in 2004. There are about 57 physicians per 100,000 people.

Health is the state of overall emotional and bodily wellbeing. Healthcare exists to provide healthiness to people and maintain their ideal conditions. In the Dominican Republic, health haphazardness has resulted in economic disgrace. It was because of the rising of infectious health disparities. Although healthcare institutions work tirelessly for the welfare of citizens, it is essential to note the prevalence of contagious diseases influences the Dominican economy.
Life expectancy in East Timor at birth was at 60.7 in 2007. The fertility rate is at six births per woman. Healthy life expectancy at birth was at 55 years in 2007.
The Human Rights Measurement Initiative finds that Suriname is fulfilling 78.4% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Suriname achieves 94.0% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 83.2% of what is expected based on the nation's level of income. Suriname falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 57.9% of what the nation is expected to achieve based on the resources (income) it has available.

In 2016, life expectancy in Tunisia was 74 years for males and 78 years for females. By comparison, in the 1960s it was only 47.1 years. Infant mortality in 2017 was 12.1 per 1,000 live births.

Health in Peru has changed drastically from pre-colonial times to the modern era. When European conquistadors invaded Peru, they brought with them diseases against which the Inca population had no acquired immunity. Much of the population died, and this marked an important turning point in the nature of Peruvian healthcare. Since Peru gained independence, the country's major healthcare concern has shifted to the disparity in care between the poor and non-poor, as well as between rural and urban populations. Another unique factor is the presence of indigenous health beliefs, which continue to be widespread in modern society.
The Health in Eswatini is poor and four years into the United Nations sustainable development goals, Eswatini seems unlikely to achieve goal on health. As a result of 63% poverty prevalence, 27% HIV prevalence, and poor health systems, maternal mortality rate is a high 389/100,000 live births, and under 5 mortality rate is 70.4/1000 live births resulting in a life expectancy that remains amongst the lowest in the world. Despite significant international aid, the government fails to adequately fund the health sector. Nurses are now and again engaged in demonstrations over poor working conditions, drug stock outs, all of which impairs quality health delivery. Despite tuberculosis and AIDS being major causes of death, diabetes and other non-communicable diseases are on the rise. Primary health care is relatively free in Eswatini save for its poor quality to meet the needs of the people. Road traffic accidents have increased over the years and they form a significant share of deaths in the country.
Life expectancy in Jamaica was 73 years in 2012.

The Human Rights Measurement Initiative finds that Maldives is fulfilling 72.0% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Maldives achieves 98.0% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves 99.7% of what is expected based on the nation's level of income. Maldives falls into the "very bad" category when evaluating the right to reproductive health because the nation is fulfilling only 18.2% of what the nation is expected to achieve based on the resources (income) it has available.