Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.

A comparison of the healthcare systems in Canada and the United States is often made by government, public health and public policy analysts. The two countries had similar healthcare systems before Canada changed its system in the 1960s and 1970s. The United States spends much more money on healthcare than Canada, on both a per-capita basis and as a percentage of GDP. In 2006, per-capita spending for health care in Canada was US$3,678; in the U.S., US$6,714. The U.S. spent 15.3% of GDP on healthcare in that year; Canada spent 10.0%. In 2006, 70% of healthcare spending in Canada was financed by government, versus 46% in the United States. Total government spending per capita in the U.S. on healthcare was 23% higher than Canadian government spending. U.S. government expenditure on healthcare was just under 83% of total Canadian spending.
The Cuban government operates a national health system and assumes fiscal and administrative responsibility for the health care of all its citizens. All healthcare in Cuba is free to Cuban residents, although challenges include low salaries for doctors, poor facilities, poor provision of equipment, and the frequent absence of essential drugs. There are no private hospitals or clinics as all health services are government-run. The current public health minister of Cuba is José Angel Portal Miranda.

Healthcare in Taiwan is administered by the Ministry of Health and Welfare of the Executive Yuan. As with other developed economies, Taiwanese people are well-nourished but face such health problems as chronic obesity and heart disease. In 2002 Taiwan had nearly 1.6 physicians and 5.9 hospital beds per 1,000 population. In 2002, there were 36 hospitals and 2,601 clinics in the country. Per capita health expenditures totaled US$752 in 2000. Health expenditures constituted 5.8 percent of the gross domestic product (GDP) in 2001 ; 64.9 percent of the expenditures were from public funds. Overall life expectancy in 2019 was averaged at 81 years.
Healthcare in Afghanistan is slowly improving after it was almost non-existent due to the decades of war. Currently, there are over 3,000 health facilities found throughout Afghanistan. More than 17,000 health posts have been established in the country, including the first neurosurgery hospital. Latest reports say 38,000 Afghan women work as midwives. From 2001 to 2021, Afghanistan experienced improvements in healthcare, with life expectancy increasing from 56 to 64 years and the maternal mortality rate reducing by 50%. 89% of residents living in cities have access to clean water in 2021, up from 16% in 2001. Despite these improvements, Afghanistan's healthcare system remains poor when compared with its neighboring countries.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, specific healthcare precincts are responsible for providing healthcare to their residents as of 2023.

In precolonial Ghana, infectious diseases were the main cause of morbidity and mortality. The modern history of health in Ghana was heavily influenced by international actors such as Christian missionaries, European colonists, the World Bank, and the International Monetary Fund. In addition, the democratic shift in Ghana spurred healthcare reforms in an attempt to address the presence of infectious and noncommunicable diseases eventually resulting in the formation of the National Health insurance Scheme in place today.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).

Hungary has a tax-funded universal healthcare system, organized by the state-owned National Health Insurance Fund. While healthcare is considered universal, several reasons persist preventing Hungarian nationals to access healthcare services. For instance, a Hungarian citizen who lived abroad but is unable to show contributions to another country's healthcare system will not be able to access the Hungarian healthcare system free of charge. However, to the OECD, 100% of the total population is covered by universal health insurance, which is absolutely free for children, mothers or fathers with babies, students, pensioners, people with low income, handicapped people, priests and other church employees. In 2022 the cost of public health insurance is 8,400 HUF per month which is the equivalent of $23.69. The healthcare system underwent significant changes which also resulted in improving life expectancy and a very low infant mortality rate. According to the OECD Hungary spent 7.8% of its GDP on health care in 2012. Total health expenditure was $US1,688.7 per capita in 2011, US$1,098.3governmental-fund (65%) and US$590.4 private-fund (35%).
The Republic of Moldova has a universal health care system.
Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance.
Research shows many health disparities among different racial and ethnic groups in the United States. Different outcomes in mental and physical health exist between all U.S. Census-recognized racial groups, but these differences stem from different historical and current factors, including genetics, socioeconomic factors, and racism. Research has demonstrated that numerous health care professionals show implicit bias in the way that they treat patients. Certain diseases have a higher prevalence among specific racial groups, and life expectancy also varies across groups.
Examples of health care systems of the world, sorted by continent, are as follows.

Lesotho's Human development index value for 2018 was 0.518—which put the country in the low human development category—positioning it at 164 out of 189 countries and territories. Health care services in Lesotho are delivered primarily by the government and the Christian Health Association of Lesotho. Access to health services is difficult for many people, especially in rural areas. The country's health system is challenged by the relentless increase of the burden of disease brought about by AIDS, and a lack of expertise and human resources. Serious emergencies are often referred to neighbouring South Africa. The largest contribution to mortality in Lesotho are communicable diseases, maternal, perinatal and nutritional conditions.

A new measure of expected human capital calculated for 195 countries from 1990 to 2016 and defined for each birth cohort as the expected years lived from age 20 to 64 years and adjusted for educational attainment, learning or education quality, and functional health status was published by The Lancet in September 2018. Latvia had the twenty-first highest level of expected human capital with 23 health, education, and learning-adjusted expected years lived between age 20 and 64 years.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.
Compared with other neighbouring countries, Guyana ranks poorly in regard to basic health indicators. Basic health services in the interior are primitive to non-existent, and some procedures are not available at all. Although Guyana's health profile falls short in comparison with many of its Caribbean neighbours, there has been remarkable progress since 1988, and the Ministry of Health is working to upgrade conditions, procedures, and facilities. Many Guyanese seek medical care in the United States, Trinidad and Tobago or Cuba.
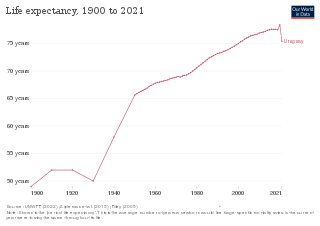
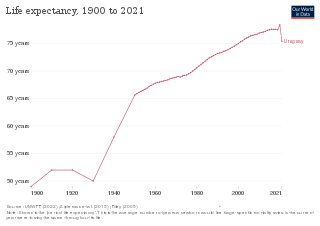
In 2016, the life expectancy in Uruguay was 73 for men and 81 for women.

Modern Mongolia inherited a relatively good healthcare system from its socialist period, a world bank report from 2007 notes "despite its low per capita income, Mongolia has relatively strong health indicators; a reflection of the important health gains achieved during the socialist period." On average Mongolia's infant mortality rate is less than half of that of similarly economically developed countries, its under-five mortality rate and life expectancy are all better on average than other nations with similar GDP per capita.

In the past, Kosovo’s capabilities to develop a modern health care system were limited. Low GDP during 1990 worsened the situation even more. However, the establishment of the Faculty of Medicine in the University of Pristina marked a significant development in health care. This was also followed by launching different health clinics which enabled better conditions for professional development.