Adaptive immune memory
Development of adaptive immune memory
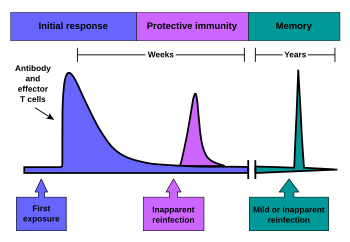
Immunological memory occurs after a primary immune response against the antigen. Immunological memory is thus created by each individual, after a previous initial exposure, to a potentially dangerous agent. The course of secondary immune response is similar to primary immune response. After the memory B cell recognizes the antigen it presents the peptide: MHC II complex to nearby effector T cells. That leads to activation of these cells and rapid proliferation of cells. After the primary immune response has disappeared, the effector cells of the immune response are eliminated. [5]
However, antibodies that were previously created in the body remain and represent the humoral component of immunological memory and comprise an important defensive mechanism in subsequent infections. In addition to the formed antibodies in the body there remains a small number of memory T and B cells that make up the cellular component of the immunological memory. They stay in blood circulation in a resting state and at the subsequent encounter with the same antigen these cells are able to respond immediately and eliminate the antigen. Memory cells have a long life and last up to several decades in the body. [6] [2]
Immunity to chickenpox, measles, and some other diseases lasts a lifetime. Immunity to many diseases eventually wears off. The immune system's response to a few diseases, such as dengue, counterproductively worsens the next infection (antibody-dependent enhancement). [7]
As of 2019, researchers are still trying to find out why some vaccines produce life-long immunity, while the effectiveness of other vaccines drops to zero in less than 30 years (for mumps) or less than six months (for H3N2 influenza). [8]
Evolution of adaptive immune memory
The evolutionary invention of memory T and B cells is widespread; however, the conditions required to develop this costly adaptation are specific. First, in order to evolve immune memory the initial molecular machinery cost must be high and will demand losses in other host characteristics. Second, middling or long lived organisms have higher chance of evolving such apparatus. The cost of this adaption increases if the host has a middling lifespan as the immune memory must be effective earlier in life. [9]
Furthermore, research models show that the environment plays an essential role in the diversity of memory cells in a population. Comparing the influence of multiple infections to a specific disease as opposed to disease diversity of an environment provide evidence that memory cell pools accrue diversity based on the number of individual pathogens exposed, even at the cost of efficiency when encountering more common pathogens. Individuals living in isolated environments such as islands have a less diverse population of memory cells, which are, however, present with sturdier immune responses. That indicates that the environment plays a large role in the evolution of memory cell populations. [10]
Previously acquired immune memory can be depleted by measles in unvaccinated children, leaving them at risk of infection by other pathogens in the years after infection. [11]
Memory B cells
Memory B cells are plasma cells that are able to produce antibodies for a long time. Unlike the naive B cells involved in the primary immune response the memory B cell response is slightly different. The memory B cell has already undergone clonal expansion, differentiation and affinity maturation, so it is able to divide multiple times faster and produce antibodies with much higher affinity (especially IgG). [1]
In contrast, the naive plasma cell is fully differentiated and cannot be further stimulated by antigen to divide or increase antibody production. Memory B cell activity in secondary lymphatic organs is highest during the first 2 weeks after infection. Subsequently, after 2 to 4 weeks its response declines. After the germinal center reaction the memory plasma cells are located in the bone marrow which is the main site of antibody production within the immunological memory. [12]
Memory T cells
Memory T cells can be both CD4+ and CD8+. These memory T cells do not require further antigen stimulation to proliferate; therefore, they do not need a signal via MHC. [13] Memory T cells can be divided into two functionally distinct groups based on the expression of the CCR7 chemokine receptor. This chemokine indicates the direction of migration into secondary lymphatic organs. Those memory T cells that do not express CCR7 (these are CCR7-) have receptors to migrate to the site of inflammation in the tissue and represent an immediate effector cell population. These cells were named memory effector T cells (TEM). After repeated stimulation they produce large amounts of IFN-γ, IL-4 and IL-5. In contrast, CCR7 + memory T cells lack proinflammatory and cytotoxic function but have receptors for lymph node migration. These cells were named central memory T cells (TCM). They effectively stimulate dendritic cells, and after repeated stimulation they are able to differentiate in CCR7- effector memory T cells. Both populations of these memory cells originate from naive T cells and remain in the body for several years after initial immunization. [14]
Experimental techniques used to study these cells include measuring antigen-stimulated cell proliferation and cytokine release, staining with peptide-MHC multimers or using an activation-induced marker (AIM) assay. [15]









