The ileum is the final section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In fish, the divisions of the small intestine are not as clear and the terms posterior intestine or distal intestine may be used instead of ileum. Its main function is to absorb vitamin B12, bile salts, and whatever products of digestion that were not absorbed by the jejunum.

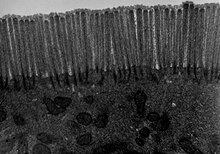
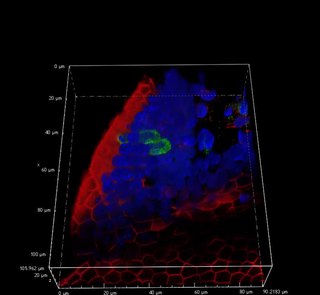
Microvilli are microscopic cellular membrane protrusions that increase the surface area for diffusion and minimize any increase in volume, and are involved in a wide variety of functions, including absorption, secretion, cellular adhesion, and mechanotransduction.

Epithelium or epithelial tissue is a thin, continuous, protective layer of compactly packed cells with little intercellular matrix. Epithelial tissues line the outer surfaces of organs and blood vessels throughout the body, as well as the inner surfaces of cavities in many internal organs. An example is the epidermis, the outermost layer of the skin. Epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. These tissues also lack blood or lymph supply. The tissue is supplied by nerves.

Tight junctions, also known as occluding junctions or zonulae occludentes, are multiprotein junctional complexes whose canonical function is to prevent leakage of solutes and water and seals between the epithelial cells. They also play a critical role maintaining the structure and permeability of endothelial cells. Tight junctions may also serve as leaky pathways by forming selective channels for small cations, anions, or water. The corresponding junctions that occur in invertebrates are septate junctions.

Caco-2 is an immortalized cell line of human colorectal adenocarcinoma cells. It is primarily used as a model of the intestinal epithelial barrier. In culture, Caco-2 cells spontaneously differentiate into a heterogeneous mixture of intestinal epithelial cells. It was developed in 1977 by Jorgen Fogh at the Sloan-Kettering Institute for Cancer Research.
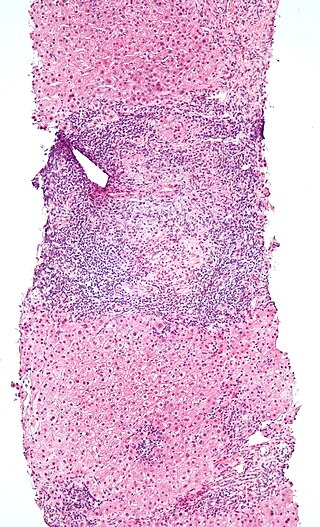
Gut-associated lymphoid tissue (GALT) is a component of the mucosa-associated lymphoid tissue (MALT) which works in the immune system to protect the body from invasion in the gut.

Paneth cells are cells in the small intestine epithelium, alongside goblet cells, enterocytes, and enteroendocrine cells. Some can also be found in the cecum and appendix. They are located below the intestinal stem cells in the intestinal glands and the large eosinophilic refractile granules that occupy most of their cytoplasm.
Intestinal permeability is a term describing the control of material passing from inside the gastrointestinal tract through the cells lining the gut wall, into the rest of the body. The intestine normally exhibits some permeability, which allows nutrients to pass through the gut, while also maintaining a barrier function to keep potentially harmful substances from leaving the intestine and migrating to the body more widely. In a healthy human intestine, small particles can migrate through tight junction claudin pore pathways, and particles up to 10–15 Å can transit through the paracellular space uptake route. There is some evidence abnormally increased intestinal permeability may play a role in some chronic diseases and inflammatory conditions. The most well understood condition with observed increased intestinal permeability is celiac disease.

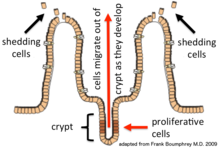
In histology, an intestinal gland is a gland found in between villi in the intestinal epithelium lining of the small intestine and large intestine. The glands and intestinal villi are covered by epithelium, which contains multiple types of cells: enterocytes, goblet cells, enteroendocrine cells, cup cells, tuft cells, and at the base of the gland, Paneth cells and stem cells.

Transcytosis is a type of transcellular transport in which various macromolecules are transported across the interior of a cell. Macromolecules are captured in vesicles on one side of the cell, drawn across the cell, and ejected on the other side. Examples of macromolecules transported include IgA, transferrin, and insulin. While transcytosis is most commonly observed in epithelial cells, the process is also present elsewhere. Blood capillaries are a well-known site for transcytosis, though it occurs in other cells, including neurons, osteoclasts and M cells of the intestine.
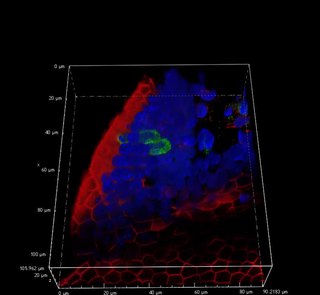
Microfold cells are found in the gut-associated lymphoid tissue (GALT) of the Peyer's patches in the small intestine, and in the mucosa-associated lymphoid tissue (MALT) of other parts of the gastrointestinal tract. These cells are known to initiate mucosal immunity responses on the apical membrane of the M cells and allow for transport of microbes and particles across the epithelial cell layer from the gut lumen to the lamina propria where interactions with immune cells can take place.
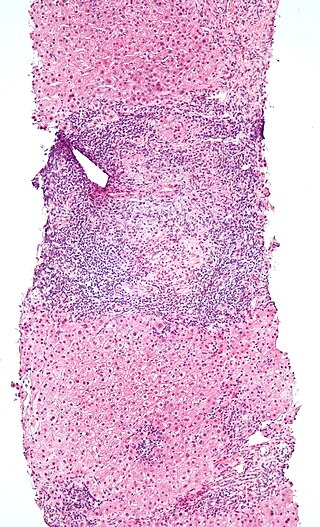
Intraepithelial lymphocytes (IEL) are lymphocytes found in the epithelial layer of mammalian mucosal linings, such as the gastrointestinal (GI) tract and reproductive tract. However, unlike other T cells, IELs do not need priming. Upon encountering antigens, they immediately release cytokines and cause killing of infected target cells. In the GI tract, they are components of gut-associated lymphoid tissue (GALT).
Paracellular transport refers to the transfer of substances across an epithelium by passing through the intercellular space between the cells. It is in contrast to transcellular transport, where the substances travel through the cell, passing through both the apical membrane and basolateral membrane.

Mucosal immunology is the study of immune system responses that occur at mucosal membranes of the intestines, the urogenital tract, and the respiratory system. The mucous membranes are in constant contact with microorganisms, food, and inhaled antigens. In healthy states, the mucosal immune system protects the organism against infectious pathogens and maintains a tolerance towards non-harmful commensal microbes and benign environmental substances. Disruption of this balance between tolerance and deprivation of pathogens can lead to pathological conditions such as food allergies, irritable bowel syndrome, susceptibility to infections, and more.
The internal surface of the uterus is lined by uterine epithelial cells which undergo dramatic changes during pregnancy. The role of the uterine epithelial cells is to selectively allow the blastocyst to implant at a specific time. All other times of the cycle, these uterine epithelial cells are refractory to blastocyst implantation. Uterine epithelial cells have a similar structure in most species and the changes which occur in the uterine epithelial cells at the time of blastocyst implantation are also conserved among most species.
Tuft cells are chemosensory cells in the epithelial lining of the intestines. Similar tufted cells are found in the respiratory epithelium where they are known as brush cells. The name "tuft" refers to the brush-like microvilli projecting from the cells. Ordinarily there are very few tuft cells present but they have been shown to greatly increase at times of a parasitic infection. Several studies have proposed a role for tuft cells in defense against parasitic infection. In the intestine, tuft cells are the sole source of secreted interleukin 25 (IL-25).
Larazotide is a synthetic eight amino acid peptide that functions as a tight junction regulator and reverses leaky junctions to their normally closed state. It is being studied in people with celiac disease.

The intestinal mucosal barrier, also referred to as intestinal barrier, refers to the property of the intestinal mucosa that ensures adequate containment of undesirable luminal contents within the intestine while preserving the ability to absorb nutrients. The separation it provides between the body and the gut prevents the uncontrolled translocation of luminal contents into the body proper. Its role in protecting the mucosal tissues and circulatory system from exposure to pro-inflammatory molecules, such as microorganisms, toxins, and antigens is vital for the maintenance of health and well-being. Intestinal mucosal barrier dysfunction has been implicated in numerous health conditions such as: food allergies, microbial infections, irritable bowel syndrome, inflammatory bowel disease, celiac disease, metabolic syndrome, non-alcoholic fatty liver disease, diabetes, and septic shock.
Tight junction proteins are molecules situated at the tight junctions of epithelial, endothelial and myelinated cells. This multiprotein junctional complex has a regulatory function in passage of ions, water and solutes through the paracellular pathway. It can also coordinate the motion of lipids and proteins between the apical and basolateral surfaces of the plasma membrane. Thereby tight junction conducts signaling molecules, that influence the differentiation, proliferation and polarity of cells. So tight junction plays a key role in maintenance of osmotic balance and trans-cellular transport of tissue specific molecules. Nowadays is known more than 40 different proteins, that are involved in these selective TJ channels.