The lungs are the central organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of the heart. Their function in the respiratory system is to extract oxygen from the air and transfer it into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere, in a process of gas exchange. The pleurae, which are thin, smooth, and moist, serve to reduce friction between the lungs and chest wall during breathing, allowing for easy and effortless movements of the lungs.

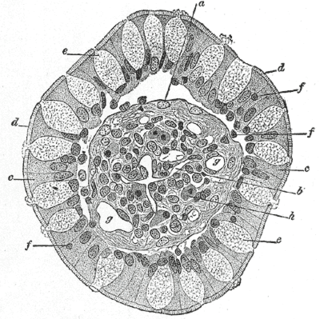
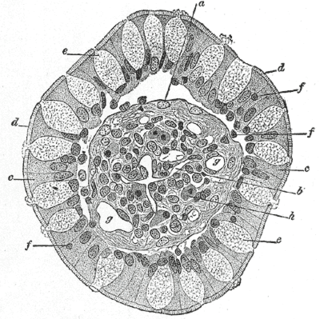
A pulmonary alveolus, also known as an air sac or air space, is one of millions of hollow, distensible cup-shaped cavities in the lungs where pulmonary gas exchange takes place. Oxygen is exchanged for carbon dioxide at the blood–air barrier between the alveolar air and the pulmonary capillary. Alveoli make up the functional tissue of the mammalian lungs known as the lung parenchyma, which takes up 90 percent of the total lung volume.

The respiratory tract is the subdivision of the respiratory system involved with the process of respiration in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.

Epithelium or epithelial tissue is a thin, continuous, protective layer of compactly packed cells with little intercellular matrix. Epithelial tissues line the outer surfaces of organs and blood vessels throughout the body, as well as the inner surfaces of cavities in many internal organs. An example is the epidermis, the outermost layer of the skin. Epithelial tissue is one of the four basic types of animal tissue, along with connective tissue, muscle tissue and nervous tissue. These tissues also lack blood or lymph supply. The tissue is supplied by nerves.

A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi to branch from the trachea at the carina are the right main bronchus and the left main bronchus. These are the widest bronchi, and enter the right lung, and the left lung at each hilum. The main bronchi branch into narrower secondary bronchi or lobar bronchi, and these branch into narrower tertiary bronchi or segmental bronchi. Further divisions of the segmental bronchi are known as 4th order, 5th order, and 6th order segmental bronchi, or grouped together as subsegmental bronchi. The bronchi, when too narrow to be supported by cartilage, are known as bronchioles. No gas exchange takes place in the bronchi.

The bronchioles or bronchioli are the smaller branches of the bronchial airways in the lower respiratory tract. They include the terminal bronchioles, and finally the respiratory bronchioles that mark the start of the respiratory zone delivering air to the gas exchanging units of the alveoli. The bronchioles no longer contain the cartilage that is found in the bronchi, or glands in their submucosa.

Mucus is a slippery aqueous secretion produced by, and covering, mucous membranes. It is typically produced from cells found in mucous glands, although it may also originate from mixed glands, which contain both serous and mucous cells. It is a viscous colloid containing inorganic salts, antimicrobial enzymes, immunoglobulins, and glycoproteins such as lactoferrin and mucins, which are produced by goblet cells in the mucous membranes and submucosal glands. Mucus serves to protect epithelial cells in the linings of the respiratory, digestive, and urogenital systems, and structures in the visual and auditory systems from pathogenic fungi, bacteria and viruses. Most of the mucus in the body is produced in the gastrointestinal tract.
Club cells, also known as bronchiolar exocrine cells, are low columnar/cuboidal cells with short microvilli, found in the small airways (bronchioles) of the lungs. They were formerly known as Clara cells.

Metaplasia is the transformation of a cell type to another cell type. The change from one type of cell to another may be part of a normal maturation process, or caused by some sort of abnormal stimulus. In simplistic terms, it is as if the original cells are not robust enough to withstand their environment, so they transform into another cell type better suited to their environment. If the stimulus causing metaplasia is removed or ceases, tissues return to their normal pattern of differentiation. Metaplasia is not synonymous with dysplasia, and is not considered to be an actual cancer. It is also contrasted with heteroplasia, which is the spontaneous abnormal growth of cytologic and histologic elements. Today, metaplastic changes are usually considered to be an early phase of carcinogenesis, specifically for those with a history of cancers or who are known to be susceptible to carcinogenic changes. Metaplastic change is thus often viewed as a premalignant condition that requires immediate intervention, either surgical or medical, lest it lead to cancer via malignant transformation.
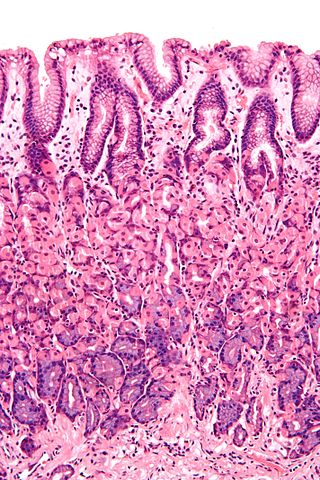
Goblet cells are simple columnar epithelial cells that secrete gel-forming mucins, like mucin 5AC. The goblet cells mainly use the merocrine method of secretion, secreting vesicles into a duct, but may use apocrine methods, budding off their secretions, when under stress. The term goblet refers to the cell's goblet-like shape. The apical portion is shaped like a cup, as it is distended by abundant mucus laden granules; its basal portion lacks these granules and is shaped like a stem.
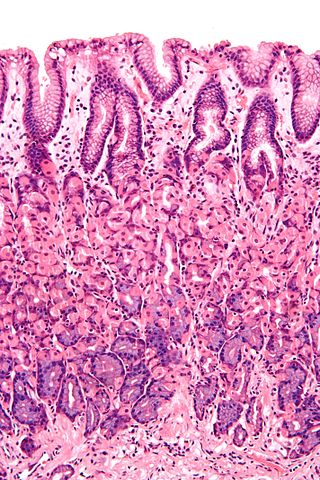
Simple columnar epithelium is a single layer of columnar epithelial cells which are tall and slender with oval-shaped nuclei located in the basal region, attached to the basement membrane. In humans, simple columnar epithelium lines most organs of the digestive tract including the stomach, and intestines. Simple columnar epithelium also lines the uterus.

Pseudostratified columnar epithelium is a type of epithelium that, though comprising only a single layer of cells, has its cell nuclei positioned in a manner suggestive of stratified columnar epithelium. A stratified epithelium rarely occurs as squamous or cuboidal.

The intestinal epithelium is the single cell layer that forms the luminal surface (lining) of both the small and large intestine (colon) of the gastrointestinal tract. Composed of simple columnar epithelium its main functions are absorption, and secretion. Useful substances are absorbed into the body, and the entry of harmful substances is restricted. Secretions include mucins, and peptides.

Mucociliary clearance (MCC), mucociliary transport, or the mucociliary escalator describes the self-clearing mechanism of the airways in the respiratory system. It is one of the two protective processes for the lungs in removing inhaled particles including pathogens before they can reach the delicate tissue of the lungs. The other clearance mechanism is provided by the cough reflex. Mucociliary clearance has a major role in pulmonary hygiene.
Histology is the study of the minute structure, composition, and function of tissues. Mature human vocal cords are composed of layered structures which are quite different at the histological level.
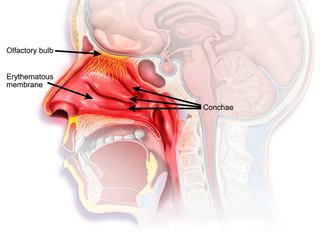
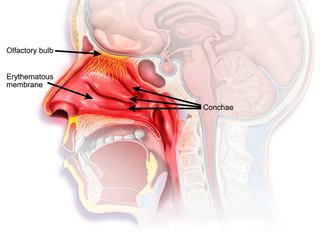
The nasal mucosa lines the nasal cavity. It is part of the respiratory mucosa, the mucous membrane lining the respiratory tract. The nasal mucosa is intimately adherent to the periosteum or perichondrium of the nasal conchae. It is continuous with the skin through the nostrils, and with the mucous membrane of the nasal part of the pharynx through the choanae. From the nasal cavity its continuity with the conjunctiva may be traced, through the nasolacrimal and lacrimal ducts; and with the frontal, ethmoidal, sphenoidal, and maxillary sinuses, through the several openings in the nasal meatuses. The mucous membrane is thickest, and most vascular, over the nasal conchae. It is also thick over the nasal septum where increased numbers of goblet cells produce a greater amount of nasal mucus. It is very thin in the meatuses on the floor of the nasal cavities, and in the various sinuses. It is one of the most commonly infected tissues in adults and children. Inflammation of this tissue may cause significant impairment of daily activities, with symptoms such as stuffy nose, headache, mouth breathing, etc.
Tuft cells are chemosensory cells in the epithelial lining of the intestines. Similar tufted cells are found in the respiratory epithelium where they are known as brush cells. The name "tuft" refers to the brush-like microvilli projecting from the cells. Ordinarily there are very few tuft cells present but they have been shown to greatly increase at times of a parasitic infection. Several studies have proposed a role for tuft cells in defense against parasitic infection. In the intestine, tuft cells are the sole source of secreted interleukin 25 (IL-25).

Anatomical terminology is used to describe microanatomical structures. This helps describe precisely the structure, layout and position of an object, and minimises ambiguity. An internationally accepted lexicon is Terminologia Histologica.

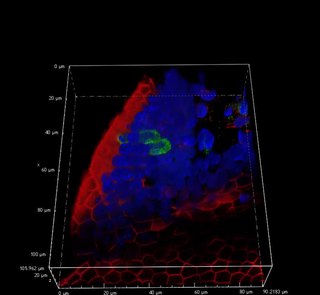
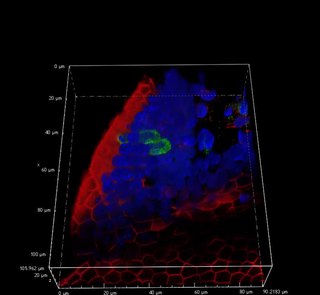
Air liquid interface cell culture (ALI) is a method of cell culture by which basal stem cells are grown with their basal surfaces in contact with media, and the top of the cellular layer is exposed to the air. The cells are then lifted and media is changed until the development of a mucociliary phenotype of a pseudostratified epithelium, similar to the tracheal epithelium.
Airway basal cells are found deep in the respiratory epithelium, attached to, and lining the basement membrane.