Warts are non-cancerous viral growths usually occurring on the hands and feet but can also affect other locations, such as the genitals or face. One or many warts may appear. They are distinguished from cancerous tumors as they are caused by a viral infection, such as a human papillomavirus, rather than a cancerous growth.

Cervical cancer is a cancer arising from the cervix or in the any layer of the wall of the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Early on, typically no symptoms are seen. Later symptoms may include abnormal vaginal bleeding, pelvic pain or pain during sexual intercourse. While bleeding after sex may not be serious, it may also indicate the presence of cervical cancer.
Human papillomavirus infection is caused by a DNA virus from the Papillomaviridae family. Many HPV infections cause no symptoms and 90% resolve spontaneously within two years. In some cases, an HPV infection persists and results in either warts or precancerous lesions. These lesions, depending on the site affected, increase the risk of cancer of the cervix, vulva, vagina, penis, anus, mouth, tonsils, or throat. Nearly all cervical cancer is due to HPV, and two strains – HPV16 and HPV18 – account for 70% of all cases. HPV16 is responsible for almost 90% of HPV-positive oropharyngeal cancers. Between 60% and 90% of the other cancers listed above are also linked to HPV. HPV6 and HPV11 are common causes of genital warts and laryngeal papillomatosis.

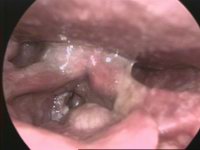
Genital warts are a sexually transmitted infection caused by certain types of human papillomavirus (HPV). They may be flat or project out from the surface of the skin, and their color may vary; brownish, white, pale yellow, pinkish-red, or gray. There may be a few individual warts or several, either in a cluster or merged together to look cauliflower-shaped. They can be itchy and feel burning. Usually they cause few symptoms, but can occasionally be painful. Typically they appear one to eight months following exposure. Warts are the most easily recognized symptom of genital HPV infection.
Laryngeal cancer or throat cancer is a kind of cancer that can develop in any part of the larynx. It is typically a squamous-cell carcinoma, reflecting its origin from the epithelium of the larynx.

Laryngitis is inflammation of the larynx. Symptoms often include a hoarse voice and may include fever, cough, pain in the front of the neck, and trouble swallowing. Typically, these last under two weeks.

Anal cancer is a cancer which arises from the anus, the distal opening of the gastrointestinal tract. Symptoms may include bleeding from the anus or a lump near the anus. Other symptoms may include pain, itchiness, or discharge from the anus. A change in bowel movements may also occur.

Head and neck cancer develops from tissues in the lip and oral cavity (mouth), larynx (throat), salivary glands, nose, sinuses, or skin of the face. The most common types of head and neck cancer occur in the lips, mouth, and larynx. Symptoms predominantly include a sore that does not heal or a change in the voice. In those with advanced disease, there may be unusual bleeding, facial pain, numbness or swelling, and visible lumps on the outside of the neck or oral cavity. Given the location of these cancers, it is possible for an afflicted individual to experience difficulty breathing.

Laryngectomy is the removal of the larynx and separation of the airway from the mouth, nose and esophagus. In a total laryngectomy, the entire larynx is removed. In a partial laryngectomy, only a portion of the larynx is removed. Following the procedure, the person breathes through an opening in the neck known as a stoma. This procedure is usually performed by an ENT surgeon in cases of laryngeal cancer. Many cases of laryngeal cancer are treated with more conservative methods. A laryngectomy is performed when these treatments fail to conserve the larynx or when the cancer has progressed such that normal functioning would be prevented. Laryngectomies are also performed on individuals with other types of head and neck cancer. Less invasive partial laryngectomies, including tracheal shaves and feminization laryngoplasty may also be performed on transgender women and other female or non-binary identified individuals to feminize the larynx and/or voice. Post-laryngectomy rehabilitation includes voice restoration, oral feeding and more recently, smell and taste rehabilitation. An individual's quality of life can be affected post-surgery.

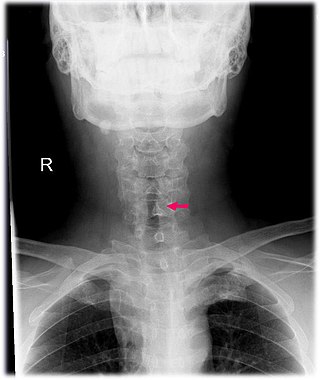
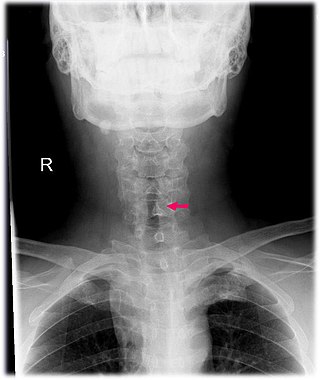
The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve that supplies all the intrinsic muscles of the larynx, with the exception of the cricothyroid muscles. There are two recurrent laryngeal nerves, right and left. The right and left nerves are not symmetrical, with the left nerve looping under the aortic arch, and the right nerve looping under the right subclavian artery then traveling upwards. They both travel alongside the trachea. Additionally, the nerves are among the few nerves that follow a recurrent course, moving in the opposite direction to the nerve they branch from, a fact from which they gain their name.

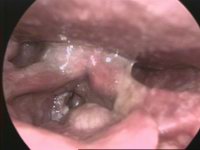
A papilloma is a benign epithelial tumor growing exophytically in nipple-like and often finger-like fronds. In this context, papilla refers to the projection created by the tumor, not a tumor on an already existing papilla.
Vocal cord paresis, also known as recurrent laryngeal nerve paralysis or vocal fold paralysis, is an injury to one or both recurrent laryngeal nerves (RLNs), which control all intrinsic muscles of the larynx except for the cricothyroid muscle. The RLN is important for speaking, breathing and swallowing.
Subglottic stenosis is a congenital or acquired narrowing of the subglottic airway. It can be congenital, acquired, iatrogenic, or very rarely, idiopathic. It is defined as the narrowing of the portion of the airway that lies between the vocal cords and the lower part of the cricoid cartilage. In a normal infant, the subglottic airway is 4.5-5.5 millimeters wide, while in a premature infant, the normal width is 3.5 millimeters. Subglottic stenosis is defined as a diameter of under 4 millimeters in an infant. Acquired cases are more common than congenital cases due to prolonged intubation being introduced in the 1960s. It is most frequently caused by certain medical procedures or external trauma, although infections and systemic diseases can also cause it.
Vaginal cancer is an extraordinarily rare form of cancer that develops in the tissue of the vagina. Primary vaginal cancer originates from the vaginal tissue – most frequently squamous cell carcinoma, but primary vaginal adenocarcinoma, sarcoma, and melanoma have also been reported – while secondary vaginal cancer involves the metastasis of a cancer that originated in a different part of the body. Secondary vaginal cancer is more common. Signs of vaginal cancer may include abnormal vaginal bleeding, dysuria, tenesmus, or pelvic pain, though as many as 20% of women diagnosed with vaginal cancer are asymptomatic at the time of diagnosis. Vaginal cancer occurs more frequently in women over age 50, and the mean age of diagnosis of vaginal cancer is 60 years. It often can be cured if found and treated in early stages. Surgery alone or surgery combined with pelvic radiation is typically used to treat vaginal cancer.

A squamous cell papilloma is a generally benign papilloma that arises from the stratified squamous epithelium of the skin, lip, oral cavity, tongue, pharynx, larynx, esophagus, cervix, vagina or anal canal. Squamous cell papillomas are typically associated with human papillomavirus (HPV) while sometimes the cause is unknown.

Laryngopharyngeal reflux (LPR) or laryngopharyngeal reflux disease (LPRD) is the retrograde flow of gastric contents into the larynx, oropharynx and/or the nasopharynx. LPR causes respiratory symptoms such as cough and wheezing and is often associated with head and neck complaints such as dysphonia, globus pharyngis, and dysphagia. LPR may play a role in other diseases, such as sinusitis, otitis media, and rhinitis, and can be a comorbidity of asthma. While LPR is commonly used interchangeably with gastroesophageal reflux disease (GERD), it presents with a different pathophysiology.
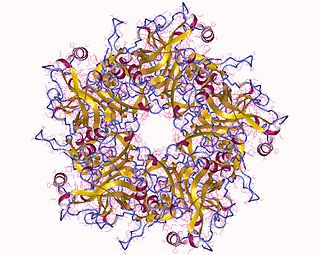
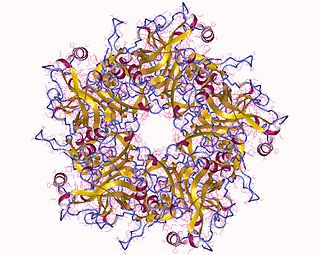
HspE7 is an investigational therapeutic vaccine candidate being developed by Nventa Biopharmaceuticals for the treatment of precancerous and cancerous lesions caused by the human papillomavirus (HPV). HspE7 uses recombinant DNA technology to covalently fuse a heat shock protein (Hsp) to a target antigen, thereby stimulating cellular immune system responses to specific diseases. HspE7 is a patented construct consisting of the HPV Type 16 E7 protein and heat shock protein 65 (Hsp65) and is currently the only candidate using Hsp technology to target the over 20 million Americans already infected with HPV.

Human papillomavirus-positive oropharyngeal cancer, is a cancer of the throat caused by the human papillomavirus type 16 virus (HPV16). In the past, cancer of the oropharynx (throat) was associated with the use of alcohol or tobacco or both, but the majority of cases are now associated with the HPV virus, acquired by having oral contact with the genitals of a person who has a genital HPV infection. Risk factors include having a large number of sexual partners, a history of oral-genital sex or anal–oral sex, having a female partner with a history of either an abnormal Pap smear or cervical dysplasia, having chronic periodontitis, and, among men, younger age at first intercourse and a history of genital warts. HPV-positive OPC is considered a separate disease from HPV-negative oropharyngeal cancer.

Bettie M. Steinberg holds multiple positions within Northwell Health: Chief Scientific Officer for The Feinstein Institute for Medical Research, Dean of the Elmezzi Graduate School of Molecular Medicine, and Chair of the Department of Molecular Medicine at the Hofstra Northwell School of Medicine in Hempstead, NY.

Squamous cell carcinoma of the vagina is a potentially invasive type of cancer that forms in the tissues of the vagina. Though uncommonly diagnosed, squamous cell cancer of the vagina (SCCV) is the most common type of vaginal cancer, accounting for 80-90% of cases as well as 2% of all gynecological cancers. SCCV forms in squamous cells, which are the thin, flat cells lining the vagina. SCCV initially spreads superficially within the vaginal wall and can slowly spread to invade other vaginal tissues. Because of its slow growth, this cancer may cause no symptoms, or it may present with signs like irregular bleeding, pain, or a vaginal mass. This carcinoma can metastasize to the lungs or less frequently to the liver, bone, or other sites. SCCV has many risk factors in common with cervical cancer and is similarly strongly associated with infection with oncogenic strains of human papillomavirus (HPV). Diagnosis of SCCV is done by pelvic exam and biopsy of the tissue. Treatment and prognosis will depend on the stage, location, and characteristics of the cancer.