Related Research Articles

A spermatozoon is a motile sperm cell, or moving form of the haploid cell that is the male gamete. A spermatozoon joins an ovum to form a zygote.
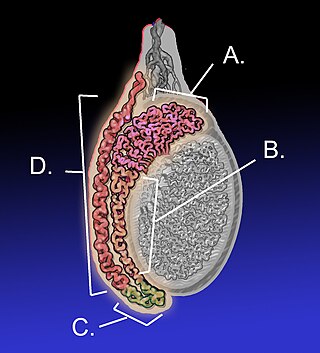
The epididymis is an elongated tubular structure attached to the posterior side of each one of the two male reproductive glands, the testicles. It is a single, narrow, tightly coiled tube in adult humans, 6 to 7 centimetres in length; uncoiled the tube would be approximately 6 m long. It connects the testicle to the vas deferens in the male reproductive system. The epididymis serves as an interconnection between the multiple efferent ducts at the rear of a testicle (proximally), and the vas deferens (distally). Its primary function is the storage, maturation and transport of sperm cells.

Azoospermia is the medical condition of a man whose semen contains no sperm. It is associated with male infertility, but many forms are amenable to medical treatment. In humans, azoospermia affects about 1% of the male population and may be seen in up to 20% of male infertility situations in Canada.
Terms oligospermia, oligozoospermia, and low sperm count refer to semen with a low concentration of sperm and is a common finding in male infertility. Often semen with a decreased sperm concentration may also show significant abnormalities in sperm morphology and motility. There has been interest in replacing the descriptive terms used in semen analysis with more quantitative information.
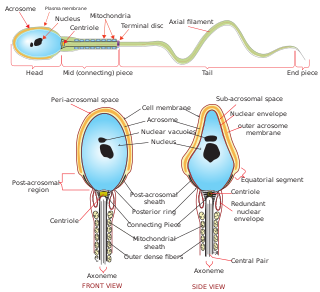
Sperm is the male reproductive cell, or gamete, in anisogamous forms of sexual reproduction. Animals produce motile sperm with a tail known as a flagellum, which are known as spermatozoa, while some red algae and fungi produce non-motile sperm cells, known as spermatia. Flowering plants contain non-motile sperm inside pollen, while some more basal plants like ferns and some gymnosperms have motile sperm.
Hypospermia is a condition in which a man has an unusually low ejaculate volume, less than 1.5 mL. It is the opposite of hyperspermia, which is a semen volume of more than 5.5 mL. It should not be confused with oligospermia, which means low sperm count. Normal ejaculate when a man is not drained from prior sex and is suitably aroused is around 1.5–6 mL, although this varies greatly with mood, physical condition, and sexual activity. Of this, around 1% by volume is sperm cells. The U.S.-based National Institutes of Health defines hypospermia as a semen volume lower than 2 mL on at least two semen analyses.
Male infertility refers to a sexually mature male's inability to impregnate a fertile female. In humans, it accounts for 40–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. More recently, advance sperm analyses that examine intracellular sperm components are being developed.
Asthenozoospermia is the medical term for reduced sperm motility. Complete asthenozoospermia, that is, 100% immotile spermatozoa in the ejaculate, is reported at a frequency of 1 of 5000 men. Causes of complete asthenozoospermia include metabolic deficiencies, ultrastructural abnormalities of the sperm flagellum and necrozoospermia.
The paternal age effect is the statistical relationship between the father's age at conception and biological effects on the child. Such effects can relate to birthweight, congenital disorders, life expectancy and psychological outcomes. A 2017 review found that while severe health effects are associated with higher paternal age, the total increase in problems caused by paternal age is low. Average paternal age at birth reached a low point between 1960 and 1980 in many countries and has been increasing since then, but has not reached historically unprecedented levels. The rise in paternal age is not seen as a major public health concern.

A semen analysis, also called seminogram or spermiogram, evaluates certain characteristics of a male's semen and the sperm contained therein. It is done to help evaluate male fertility, whether for those seeking pregnancy or verifying the success of vasectomy. Depending on the measurement method, just a few characteristics may be evaluated or many characteristics may be evaluated. Collection techniques and precise measurement method may influence results. The assay is also referred to as ejaculate analysis, human sperm assay (HSA), sperm function test, and sperm assay.
Semen quality is a measure of male fertility, a measure of the ability of sperm in semen to accomplish fertilization. Semen quality involves both sperm quantity and quality. Semen quality is a major factor for fertility.

In human anatomy, the penis is an external male sex organ that additionally serves as the urinary duct. The main parts are the root, body, the epithelium of the penis including the shaft skin, and the foreskin covering the glans. The body of the penis is made up of three columns of tissue: two corpora cavernosa on the dorsal side and corpus spongiosum between them on the ventral side. The urethra passes through the prostate gland, where it is joined by the ejaculatory duct, and then through the penis. The urethra goes across the corpus spongiosum and ends at the tip of the glans as the opening, the urinary meatus. It is a passage both for excretion of urine and the ejaculation of semen.

Sperm motility describes the ability of sperm to move properly through the female reproductive tract or through water to reach the egg. Sperm motility can also be thought of as the quality, which is a factor in successful conception; sperm that do not "swim" properly will not reach the egg in order to fertilize it. Sperm motility in mammals also facilitates the passage of the sperm through the cumulus oophorus and the zona pellucida, which surround the mammalian oocyte.
Sperm sorting is a means of choosing what type of sperm cell is to fertilize the egg cell. Several conventional techniques of centrifugation or swim-up. Newly applied methods such as flow cytometry expand the possibilities of sperm sorting and new techniques of sperm sorting are being developed.
Semen cryopreservation is a procedure to preserve sperm cells. Semen can be used successfully indefinitely after cryopreservation. It can be used for sperm donation where the recipient wants the treatment in a different time or place, or as a means of preserving fertility for men undergoing vasectomy or treatments that may compromise their fertility, such as chemotherapy, radiation therapy or surgery. It is also often used by trans women prior to medically transitioning in ways that affect fertility, such as feminizing hormone therapy and orchiectomies.
Testicular dysgenesis syndrome is a male reproduction-related condition characterized by the presence of symptoms and disorders such as hypospadias, cryptorchidism, poor semen quality, and testicular cancer. The concept was first introduced by N.E. Skakkaebaek in a research paper along with the department of Growth and Reproduction in Copenhagen University. The paper suggests the origin and underlying cause of TDS can be detected as early as in fetal life, where environmental and genomic factors could affect the development of the male reproductive system.
Obesity is defined as an abnormal accumulation of body fat, usually 20% or more over an individual's ideal body weight. This is often described as a body mass index (BMI) over 30. However, BMI does not account for whether the excess weight is fat or muscle, and is not a measure of body composition. For most people, however, BMI is an indication used worldwide to estimate nutritional status. Obesity is usually the result of consuming more calories than the body needs and not expending that energy by doing exercise. There are genetic causes and hormonal disorders that cause people to gain significant amounts of weight but this is rare. People in the obese category are much more likely to suffer from fertility problems than people of normal healthy weight.
Antisperm antibodies (ASA) are antibodies produced against sperm antigens.
The male infertility crisis is an increase in male infertility since the mid-1970s. The issue attracted media attention after a 2017 meta-analysis found that sperm counts had declined by 52.4 percent between 1973 and 2011. The decline is particularly prevalent in Western countries such as New Zealand, Australia, Europe, and North America. A 2022 meta-analysis reported that this decline extends to non-Western countries, namely those in Asia, Africa, Central America, and South America. This meta-analysis also suggests that the decline in sperm counts may be accelerating.

Sperm Chromatin Structure Assay (SCSA) is a diagnostic approach that detects sperm abnormality with a large extent of DNA fragmentation. First described by Evenson in 1980, the assay is a flow cytometric test that detects the vulnerability of sperm DNA to acid-induced denaturation DNA in situ. SCSA measures sperm DNA fragmentation attributed to intrinsic and extrinsic factors and reports the degree of fragmentation in terms of DNA Fragmentation Index (DFI). The use of SCSA expands from evaluation of male infertility and subfertility, toxicology studies and evaluation of quality of laboratory semen samples. Notably, SCSA outcompetes other convention sperm DNA fragmentation (sDF) assays such as TUNEL and COMET in terms of efficiency, objectivity, and repeatability.
References
- ↑ World Health Organization (WHO) Laboratory Manual for the Examination and Processing of Human Semen, 5th Edition, 2010
- ↑ Lecomte PJ, Barthelemy C., Nduwayo L., Hamamah S. (1999) Necrospermia: Etiology and treatment. In: Hamamah S., Olivennes F., Mieusset R., Frydman R. (eds) Male Sterility and Motility Disorders. Serono Symposia USA. Springer, New York, NY. https://doi.org/10.1007/978-1-4612-1522-6_6
- ↑ Doddamani SH, Shubhashree MN, Giri SK, Naik R, Bharali BK (January–March 2019). "Ayurvedic management of necrozoospermia - A case report". AYU. 40 (1): 44–47. doi: 10.4103/ayu.AYU_120_15 . PMC 6891995 . PMID 31831968.