The salivary glands in many vertebrates including mammals are exocrine glands that produce saliva through a system of ducts. Humans have three paired major salivary glands, as well as hundreds of minor salivary glands. Salivary glands can be classified as serous, mucous, or seromucous (mixed).
Articles related to anatomy include:

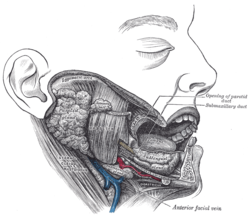
The parotid gland is a major salivary gland in many animals. In humans, the two parotid glands are present on either side of the mouth and in front of both ears. They are the largest of the salivary glands. Each parotid is wrapped around the mandibular ramus, and secretes serous saliva through the parotid duct into the mouth, to facilitate mastication and swallowing and to begin the digestion of starches. There are also two other types of salivary glands; they are submandibular and sublingual glands. Sometimes accessory parotid glands are found close to the main parotid glands.

The paired submandibular glands are major salivary glands located beneath the floor of the mouth. In adult humans, they each weigh about 15 grams and contribute some 60–67% of unstimulated saliva secretion; on stimulation their contribution decreases in proportion as parotid gland secretion rises to 50%. The average length of the normal adult human submandibular salivary gland is approximately 27 mm, while the average width is approximately 14.3 mm.

The sublingual gland is a seromucous polystomatic exocrine gland. Located underneath the oral diaphragm, the sublingual gland is the smallest and most diffuse of the three major salivary glands of the oral cavity, with the other two being the submandibular and parotid. The sublingual gland provides approximately 3-5% of the total salivary volume.

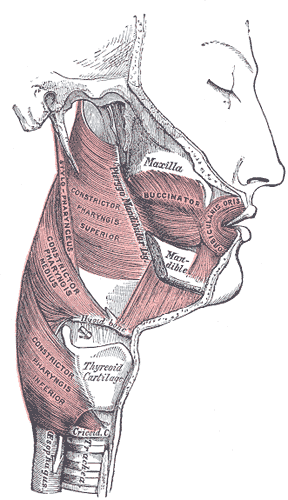
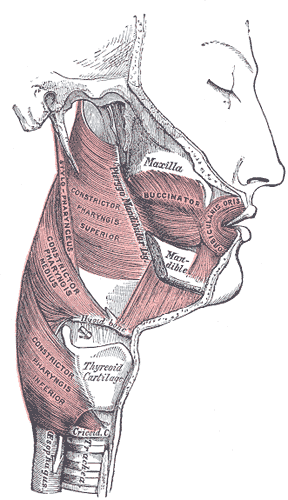
The buccinator is a thin quadrilateral muscle occupying the interval between the maxilla and the mandible at the side of the face. It forms the anterior part of the cheek or the lateral wall of the oral cavity.

Parotitis is an inflammation of one or both parotid glands, the major salivary glands located on either side of the face, in humans. The parotid gland is the salivary gland most commonly affected by inflammation.

The facial artery is a branch of the external carotid artery that supplies structures of the superficial face.

The buccal nerve is a sensory nerve of the face arising from the mandibular nerve. It conveys sensory information from the skin of the cheek, and parts of the oral mucosa, periodontium, and gingiva.

The transverse facial artery is an artery that branches from the superficial temporal artery and runs across the face.

The masseteric fascia and parotideomasseteric fascia are fascias of the head varyingly described depending upon the source consulted. They may or may not be described as one and the same structure.

Sialadenitis (sialoadenitis) is inflammation of salivary glands, usually the major ones, the most common being the parotid gland, followed by submandibular and sublingual glands. It should not be confused with sialadenosis (sialosis) which is a non-inflammatory enlargement of the major salivary glands.

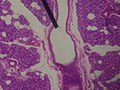
Sialolithiasis is a crystallopathy where a calcified mass or sialolith forms within a salivary gland, usually in the duct of the submandibular gland. Less commonly the parotid gland or rarely the sublingual gland or a minor salivary gland may develop salivary stones.

This article describes the anatomy of the head and neck of the human body, including the brain, bones, muscles, blood vessels, nerves, glands, nose, mouth, teeth, tongue, and throat.
The buccal space is a fascial space of the head and neck. It is a potential space in the cheek, and is paired on each side. The buccal space is superficial to the buccinator muscle and deep to the platysma muscle and the skin. The buccal space is part of the subcutaneous space, which is continuous from head to toe.

In anatomy and physiology, a duct is a circumscribed channel leading from an exocrine gland or organ.
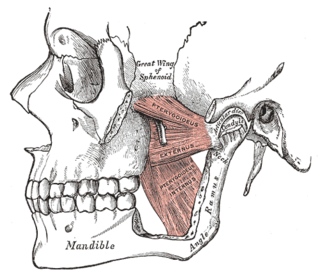
Inferior alveolar nerve block is a nerve block technique which induces anesthesia (numbness) in the areas of the mouth and face innervated by one of the inferior alveolar nerves which are paired on the left and right side. These areas are the skin and mucous membranes of the lower lip, the skin of the chin, the lower teeth and the labial gingiva of the anterior teeth, all unilaterally to the midline of the side on which the block is administered. However, depending on technique, the long buccal nerve may not be anesthetized by an IANB and therefore an area of buccal gingiva adjacent to the lower posterior teeth will retain normal sensation unless that nerve is anesthetized separately, via a (long) buccal nerve block. The inferior alveolar nerve is a branch of the mandibular nerve, the third division of the trigeminal nerve. This procedure attempts to anaesthetise the inferior alveolar nerve prior to it entering the mandibular foramen on the medial surface of the mandibular ramus.
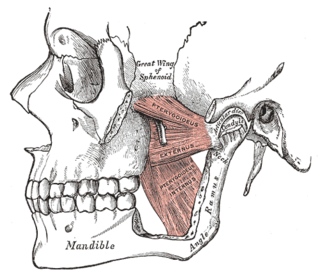
The pterygomandibular space is a fascial space of the head and neck. It is a potential space in the head and is paired on each side. It is located between the lateral pterygoid muscle and the medial surface of the ramus of the mandible. The pterygomandibular space is one of the four compartments of the masticator space.

Salivary gland diseases (SGDs) are multiple and varied in cause. There are three paired major salivary glands in humans: the parotid glands, the submandibular glands, and the sublingual glands. There are also about 800–1,000 minor salivary glands in the mucosa of the mouth. The parotid glands are in front of the ears, one on side, and secrete mostly serous saliva, via the parotid ducts, into the mouth, usually opening roughly opposite the second upper molars. The submandibular gland is medial to the angle of the mandible, and it drains its mixture of serous and mucous saliva via the submandibular duct into the mouth, usually opening in a punctum in the floor of mouth. The sublingual gland is below the tongue, on the floor of the mouth; it drains its mostly mucous saliva into the mouth via about 8–20 ducts, which open along the plica sublingualis, a fold of tissue under the tongue.
Pneumoparotitis, is a rare cause of parotid gland swelling which occurs when air is forced through the parotid (Stensen) duct resulting in inflation of the duct.