Human teeth function to mechanically break down items of food by cutting and crushing them in preparation for swallowing and digesting. As such, they are considered part of the human digestive system. Humans have four types of teeth: incisors, canines, premolars, and molars, which each have a specific function. The incisors cut the food, the canines tear the food and the molars and premolars crush the food. The roots of teeth are embedded in the maxilla or the mandible and are covered by gums. Teeth are made of multiple tissues of varying density and hardness.

Tooth enamel is one of the four major tissues that make up the tooth in humans and many animals, including some species of fish. It makes up the normally visible part of the tooth, covering the crown. The other major tissues are dentin, cementum, and dental pulp. It is a very hard, white to off-white, highly mineralised substance that acts as a barrier to protect the tooth but can become susceptible to degradation, especially by acids from food and drink. In rare circumstances enamel fails to form, leaving the underlying dentin exposed on the surface.

Dentin or dentine is a calcified tissue of the body and, along with enamel, cementum, and pulp, is one of the four major components of teeth. It is usually covered by enamel on the crown and cementum on the root and surrounds the entire pulp. By volume, 45% of dentin consists of the mineral hydroxyapatite, 33% is organic material, and 22% is water. Yellow in appearance, it greatly affects the color of a tooth due to the translucency of enamel. Dentin, which is less mineralized and less brittle than enamel, is necessary for the support of enamel. Dentin rates approximately 3 on the Mohs scale of mineral hardness. There are two main characteristics which distinguish dentin from enamel: firstly, dentin forms throughout life; secondly, dentin is sensitive and can become hypersensitive to changes in temperature due to the sensory function of odontoblasts, especially when enamel recedes and dentin channels become exposed.

The periodontium is the specialized tissues that both surround and support the teeth, maintaining them in the maxillary and mandibular bones. The word comes from the Greek terms περί peri-, meaning "around" and -odont, meaning "tooth". Literally taken, it means that which is "around the tooth". Periodontics is the dental specialty that relates specifically to the care and maintenance of these tissues. It provides the support necessary to maintain teeth in function. It consists of four principal components, namely:

Cementoenamel junction (CEJ) is defined as the area of the union of cementum and enamel at the cervical region of the tooth. It is a slightly visible anatomical border identified on a tooth. It is the location where the enamel, which covers the anatomical crown of a tooth, and the cementum, which covers the anatomical root of a tooth, meet. Informally it is known as the neck of the tooth. The border created by these two dental tissues has much significance as it is usually the location where the gingiva attaches to a healthy tooth by fibers called the gingival fibers.

The periodontal ligament, commonly abbreviated as the PDL, are a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which they sit. It inserts into root cementum on one side and onto alveolar bone on the other.
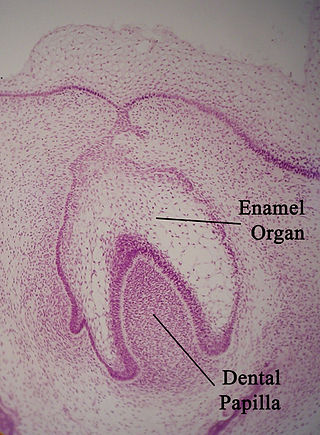
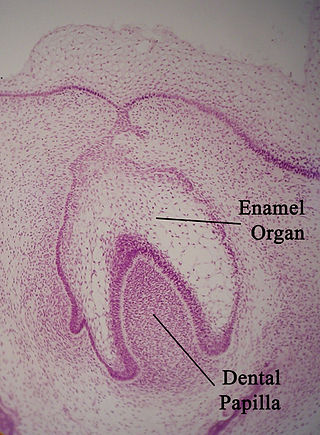
The enamel organ, also known as the dental organ, is a cellular aggregation seen in a developing tooth and it lies above the dental papilla. The enamel organ which is differentiated from the primitive oral epithelium lining the stomodeum. The enamel organ is responsible for the formation of enamel, initiation of dentine formation, establishment of the shape of a tooth's crown, and establishment of the dentoenamel junction.

Tooth development or odontogenesis is the complex process by which teeth form from embryonic cells, grow, and erupt into the mouth. For human teeth to have a healthy oral environment, all parts of the tooth must develop during appropriate stages of fetal development. Primary (baby) teeth start to form between the sixth and eighth week of prenatal development, and permanent teeth begin to form in the twentieth week. If teeth do not start to develop at or near these times, they will not develop at all, resulting in hypodontia or anodontia.

In embryology and prenatal development, the dental papilla is a condensation of ectomesenchymal cells called odontoblasts, seen in histologic sections of a developing tooth. It lies below a cellular aggregation known as the enamel organ. The dental papilla appears after 8–10 weeks intra uteral life. The dental papilla gives rise to the dentin and pulp of a tooth.

In vertebrates, an odontoblast is a cell of neural crest origin that is part of the outer surface of the dental pulp, and whose biological function is dentinogenesis, which is the formation of dentin, the substance beneath the tooth enamel on the crown and the cementum on the root.
Periodontology or periodontics is the specialty of dentistry that studies supporting structures of teeth, as well as diseases and conditions that affect them. The supporting tissues are known as the periodontium, which includes the gingiva (gums), alveolar bone, cementum, and the periodontal ligament. A periodontist is a dentist that specializes in the prevention, diagnosis and treatment of periodontal disease and in the placement of dental implants.

The dental follicle, also known as dental sac, is made up of mesenchymal cells and fibres surrounding the enamel organ and dental papilla of a developing tooth. It is a vascular fibrous sac containing the developing tooth and its odontogenic organ. The dental follicle (DF) differentiates into the periodontal ligament. In addition, it may be the precursor of other cells of the periodontium, including osteoblasts, cementoblasts and fibroblasts. They develop into the alveolar bone, the cementum with Sharpey's fibers and the periodontal ligament fibers respectively. Similar to dental papilla, the dental follicle provides nutrition to the enamel organ and dental papilla and also have an extremely rich blood supply.

The Hertwig epithelial root sheath (HERS) or epithelial root sheath is a proliferation of epithelial cells located at the cervical loop of the enamel organ in a developing tooth. Hertwig epithelial root sheath initiates the formation of dentin in the root of a tooth by causing the differentiation of odontoblasts from the dental papilla. The root sheath eventually disintegrates with the periodontal ligament, but residual pieces that do not completely disappear are seen as epithelial cell rests of Malassez (ERM). These rests can become cystic, presenting future periodontal infections.
Cementogenesis is the formation of cementum, one of the three mineralized substances of a tooth. Cementum covers the roots of teeth and serves to anchor gingival and periodontal fibers of the periodontal ligament by the fibers to the alveolar bone.

The gingival sulcus is an area of potential space between a tooth and the surrounding gingival tissue and is lined by sulcular epithelium. The depth of the sulcus is bounded by two entities: apically by the gingival fibers of the connective tissue attachment and coronally by the free gingival margin. A healthy sulcular depth is three millimeters or less, which is readily self-cleansable with a properly used toothbrush or the supplemental use of other oral hygiene aids.
Dental anatomy is a field of anatomy dedicated to the study of human tooth structures. The development, appearance, and classification of teeth fall within its purview. Tooth formation begins before birth, and the teeth's eventual morphology is dictated during this time. Dental anatomy is also a taxonomical science: it is concerned with the naming of teeth and the structures of which they are made, this information serving a practical purpose in dental treatment.
The junctional epithelium (JE) is that epithelium which lies at, and in health also defines, the base of the gingival sulcus. The probing depth of the gingival sulcus is measured by a calibrated periodontal probe. In a healthy-case scenario, the probe is gently inserted, slides by the sulcular epithelium (SE), and is stopped by the epithelial attachment (EA). However, the probing depth of the gingival sulcus may be considerably different from the true histological gingival sulcus depth.
In dentistry, enamel matrix derivative (EMD) is an extract of porcine fetal tooth material used to biomimetically stimulate the soft and hard tissues surrounding teeth to regrow following tissue destruction.
Hard tissue, refers to "normal" calcified tissue, is the tissue which is mineralized and has a firm intercellular matrix. The hard tissues of humans are bone, tooth enamel, dentin, and cementum. The term is in contrast to soft tissue.
A cementicle is a small, spherical or ovoid calcified mass embedded within or attached to the cementum layer on the root surface of a tooth, or lying free within the periodontal ligament. They tend to occur in elderly individuals.