Leprosy, also known as Hansen's disease (HD), is a long-term infection by the bacteria Mycobacterium leprae or Mycobacterium lepromatosis. Infection can lead to damage of the nerves, respiratory tract, skin, and eyes. This nerve damage may result in a lack of ability to feel pain, which can lead to the loss of parts of a person's extremities from repeated injuries or infection through unnoticed wounds. An infected person may also experience muscle weakness and poor eyesight. Leprosy symptoms may begin within one year, but, for some people, symptoms may take 20 years or more to occur.
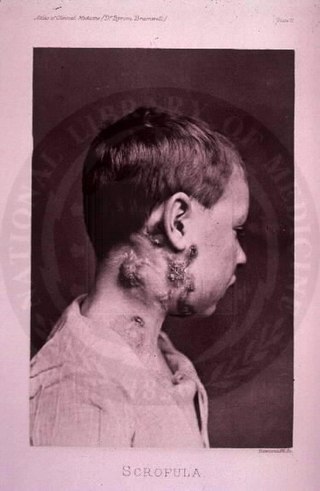
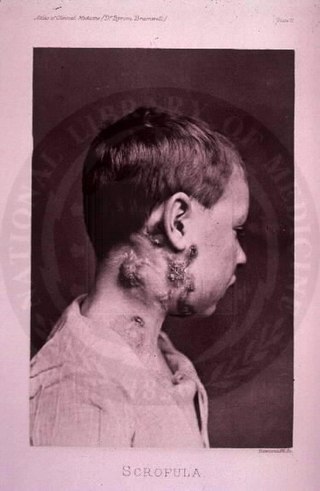
The disease mycobacterial cervical lymphadenitis, also known as scrofula and historically as king's evil, involves a lymphadenitis of the cervical lymph nodes associated with tuberculosis as well as nontuberculous (atypical) mycobacteria.

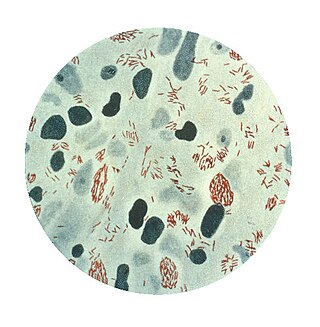
Mycobacterium tuberculosis, also known as Koch's bacillus, is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis. First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear weakly Gram-positive. Acid-fast stains such as Ziehl–Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs. The most frequently used diagnostic methods for tuberculosis are the tuberculin skin test, acid-fast stain, culture, and polymerase chain reaction.

Mycobacterium is a genus of over 190 species in the phylum Actinomycetota, assigned its own family, Mycobacteriaceae. This genus includes pathogens known to cause serious diseases in mammals, including tuberculosis and leprosy in humans. The Greek prefix myco- means 'fungus', alluding to this genus' mold-like colony surfaces. Since this genus has cell walls with a waxy lipid-rich outer layer that contains high concentrations of mycolic acid, acid-fast staining is used to emphasize their resistance to acids, compared to other cell types.
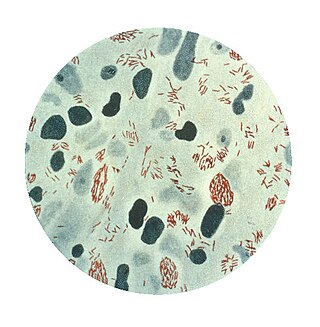
Mycobacterium leprae is one of the two species of bacteria that cause Hansen's disease (leprosy), a chronic but curable infectious disease that damages the peripheral nerves and targets the skin, eyes, nose, and muscles.
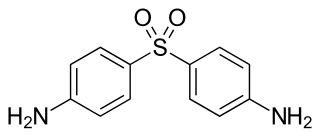
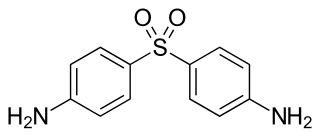
Dapsone, also known as 4,4'-sulfonyldianiline (SDA) or diaminodiphenyl sulfone (DDS), is an antibiotic commonly used in combination with rifampicin and clofazimine for the treatment of leprosy. It is a second-line medication for the treatment and prevention of pneumocystis pneumonia and for the prevention of toxoplasmosis in those who have poor immune function. Additionally, it has been used for acne, dermatitis herpetiformis, and various other skin conditions. Dapsone is available both topically and by mouth.
Nontuberculous mycobacteria (NTM), also known as environmental mycobacteria, atypical mycobacteria and mycobacteria other than tuberculosis (MOTT), are mycobacteria which do not cause tuberculosis or leprosy/Hansen's disease. NTM are able to cause pulmonary diseases that resemble tuberculosis. Mycobacteriosis is any of these illnesses, usually meant to exclude tuberculosis. They occur in many animals, including humans and are commonly found in soil and water.

Rifampicin, also known as rifampin, is an ansamycin antibiotic used to treat several types of bacterial infections, including tuberculosis (TB), Mycobacterium avium complex, leprosy, and Legionnaires' disease. It is almost always used together with other antibiotics with two notable exceptions: when given as a "preferred treatment that is strongly recommended" for latent TB infection; and when used as post-exposure prophylaxis to prevent Haemophilus influenzae type b and meningococcal disease in people who have been exposed to those bacteria. Before treating a person for a long period of time, measurements of liver enzymes and blood counts are recommended. Rifampicin may be given either by mouth or intravenously.

In organic chemistry, a sulfone is a organosulfur compound containing a sulfonyl functional group attached to two carbon atoms. The central hexavalent sulfur atom is double-bonded to each of two oxygen atoms and has a single bond to each of two carbon atoms, usually in two separate hydrocarbon substituents.

Erythema nodosum (EN) is an inflammatory condition characterized by inflammation of the fat cells under the skin, resulting in tender red nodules or lumps that are usually seen on both shins. It can be caused by a variety of conditions, and typically resolves spontaneously within 30 days. It is common in young people aged 12–20 years.

Clofazimine, sold under the brand name Lamprene, is a medication used together with rifampicin and dapsone to treat leprosy. It is specifically used for multibacillary (MB) leprosy and erythema nodosum leprosum. Evidence is insufficient to support its use in other conditions though a retrospective study found it 95% effective in the treatment of Mycobacterium avium complex (MAC) when administered with a macrolide and ethambutol, as well as the drugs amikacin and clarithromycin. However, in the United States, clofazimine is considered an orphan drug, is unavailable in pharmacies, and its use in the treatment of MAC is overseen by the Food and Drug Administration. It is taken orally.

Mycobacterium avium-intracellulare infection (MAI) is an atypical mycobacterial infection, i.e. one with nontuberculous mycobacteria or NTM, caused by Mycobacterium avium complex (MAC), which is made of two Mycobacterium species, M. avium and M. intracellulare. This infection causes respiratory illness in birds, pigs, and humans, especially in immunocompromised people. In the later stages of AIDS, it can be very severe. It usually first presents as a persistent cough. It is typically treated with a series of three antibiotics for a period of at least six months.

Mycobacterium kansasii is a bacterium in the Mycobacterium genus. It is an environmental bacteria that causes opportunistic infections in humans, and is one of the leading mycobacterial causes of human disease after tuberculosis and leprosy.

Acedapsone (INN) is an antimicrobial drug, which also has antimalarial activity.
A leprostatic agent is a drug that interferes with proliferation of the bacterium that causes leprosy.

Lepromatous leprosy is a form of leprosy characterized by pale macules in the skin.
Guy Henry Faget (1891–1947) was an American medical doctor who revolutionalized the treatment of leprosy, by demonstrating the efficacy of promin, as described in a paper published in 1943. Promin is a sulfone compound, synthesized by Feldman and his co-workers in 1940, which is a chemotherapeutic agent that was determined to be effective against tuberculosis in experimental animals. He was the grandson of Jean Charles Faget, and father of Maxime Faget.
Hydnocarpus wightianus or chaulmoogra is a tree in the Achariaceae family. Hydnocarpus wightiana seed oil has been widely used in traditional Indian medicine, especially in Ayurveda, and in Chinese traditional medicine for the treatment of leprosy. It entered early Western medicine in the nineteenth century before the era of sulfonamides and other antibiotics for the treatment of several skin diseases and leprosy. The oil was prescribed for leprosy as a mixture suspended in gum or as an emulsion.

The history of leprosy was traced to its origins by an international team of 22 geneticists using comparative genomics of the worldwide distribution of Mycobacterium leprae. Monot et al. (2005) determined that leprosy originated in East Africa or the Near East and traveled with humans along their migration routes, including those of trade in goods and slaves. The four strains of M. leprae are based in specific geographic regions where each predominantly occurs:

Lalita Ramakrishnan is an Indian-born American microbiologist who is known for her contributions to the understanding of the biological mechanism of tuberculosis. As of 2019 she serves as a professor of Immunology and Infectious Diseases at the University of Cambridge, where she is also a Wellcome Trust Principal Research Fellow and a practicing physician. Her research is conducted at the MRC Laboratory of Molecular Biology, where she serves as the Head of the Molecular Immunity Unit of the Department of Medicine embedded at the MRC LMB. Working with Stanley Falkow at Stanford, she developed the strategy of using Mycobacterium marinum infection as a model for tuberculosis. Her work has appeared in a number of journals, including Science, Nature, and Cell. In 2018 and 2019 Ramakrishnan coauthored two influential papers in the British Medical Journal (BMJ) arguing that the widely accepted estimates of the prevalence of latent tuberculosis—estimates used as a basis for allocation of research funds—are far too high. She is married to Mark Troll, a physical chemist.