Related Research Articles

Kikuchi disease was described in 1972 in Japan. It is also known as histiocytic necrotizing lymphadenitis, Kikuchi necrotizing lymphadenitis, phagocytic necrotizing lymphadenitis, subacute necrotizing lymphadenitis, and necrotizing lymphadenitis. Kikuchi disease occurs sporadically in people with no family history of the condition.
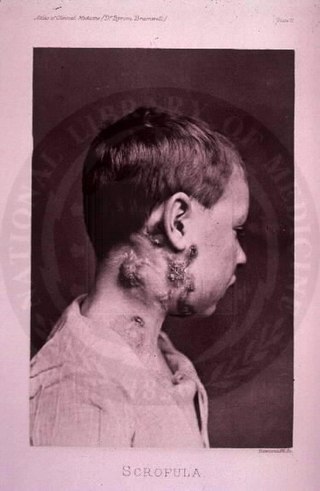
The disease mycobacterial cervical lymphadenitis, also known as scrofula and historically as king's evil, involves a lymphadenitis of the cervical lymph nodes associated with tuberculosis as well as nontuberculous (atypical) mycobacteria.

A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious organisms including bacteria and fungi, as well as other materials such as foreign objects, keratin, and suture fragments.
Adenitis is a general term for an inflammation of a gland. Often it is used to refer to lymphadenitis which is the inflammation of a lymph node.
Nontuberculous mycobacteria (NTM), also known as environmental mycobacteria, atypical mycobacteria and mycobacteria other than tuberculosis (MOTT), are mycobacteria which do not cause tuberculosis or leprosy. NTM do cause pulmonary diseases that resemble tuberculosis. Mycobacteriosis is any of these illnesses, usually meant to exclude tuberculosis. They occur in many animals, including humans and are commonly found in soil and water.

Lymphadenopathy or adenopathy is a disease of the lymph nodes, in which they are abnormal in size or consistency. Lymphadenopathy of an inflammatory type is lymphadenitis, producing swollen or enlarged lymph nodes. In clinical practice, the distinction between lymphadenopathy and lymphadenitis is rarely made and the words are usually treated as synonymous. Inflammation of the lymphatic vessels is known as lymphangitis. Infectious lymphadenitis affecting lymph nodes in the neck is often called scrofula.

Caseous necrosis or caseous degeneration is a unique form of cell death in which the tissue maintains a cheese-like appearance. It is also a distinctive form of coagulative necrosis. The dead tissue appears as a soft and white proteinaceous dead cell mass.

Miliary tuberculosis is a form of tuberculosis that is characterized by a wide dissemination into the human body and by the tiny size of the lesions (1–5 mm). Its name comes from a distinctive pattern seen on a chest radiograph of many tiny spots distributed throughout the lung fields with the appearance similar to millet seeds—thus the term "miliary" tuberculosis. Miliary TB may infect any number of organs, including the lungs, liver, and spleen. Miliary tuberculosis is present in about 2% of all reported cases of tuberculosis and accounts for up to 20% of all extra-pulmonary tuberculosis cases.
The CDC Classification System for HIV Infection is the medical classification system used by the United States Centers for Disease Control and Prevention (CDC) to classify HIV disease and infection. The system is used to allow the government to handle epidemic statistics and define who receives US government assistance.

A giant cell is a mass formed by the union of several distinct cells, often forming a granuloma.

Lupus vulgaris are painful cutaneous tuberculosis skin lesions with nodular appearance, most often on the face around the nose, eyelids, lips, cheeks, ears and neck. It is the most common Mycobacterium tuberculosis skin infection. The lesions may ultimately develop into disfiguring skin ulcers if left untreated.

Mycobacterium avium-intracellulare infection (MAI) is an atypical mycobacterial infection, i.e. one with nontuberculous mycobacteria or NTM, caused by Mycobacterium avium complex (MAC), which is made of two Mycobacterium species, M. avium and M. intracellulare. This infection causes respiratory illness in birds, pigs, and humans, especially in immunocompromised people. In the later stages of AIDS, it can be very severe. It usually first presents as a persistent cough. It is typically treated with a series of three antibiotics for a period of at least six months.

Ghon's complex is a lesion seen in the lung that is caused by tuberculosis. The lesions consist of a Ghon focus along with pulmonary lymphadenopathy within a nearby pulmonary lymph node. A Ghon's complex retains viable bacteria, making them sources of long-term infection, which may reactivate and trigger secondary tuberculosis later in life.

Langhans giant cells (LGC) are giant cells found in granulomatous conditions.
Orofacial granulomatosis (OFG) is a condition characterized by persistent enlargement of the soft tissues of the mouth, lips and the area around the mouth on the face, causing in most cases extreme pain. The mechanism of the enlargement is granulomatous inflammation. The underlying cause of the condition is not completely understood, and there is disagreement as to how it relates to Crohn's disease and sarcoidosis.

According to a common point of view epithelioid cells are derivatives of activated macrophages resembling epithelial cells.

Cervical lymphadenopathy refers to lymphadenopathy of the cervical lymph nodes. The term lymphadenopathy strictly speaking refers to disease of the lymph nodes, though it is often used to describe the enlargement of the lymph nodes. Similarly, the term lymphadenitis refers to inflammation of a lymph node, but often it is used as a synonym of lymphadenopathy.

Caseous lymphadenitis (CLA) is an infectious disease caused by the bacterium Corynebacterium pseudotuberculosis, that affects the lymphatic system, resulting in abscesses in the lymph nodes and internal organs. It is found mostly in goats and sheep and at the moment it has no cure.
Corynebacterium pseudotuberculosis is a Gram-positive bacterium known to infect ruminants, horses, and rarely people. It is a facultative anaerobic organism that is catalase-positive and capable of beta-hemolysis. In small ruminants, C. pseudotuberculosis causes a disease called caseous lymphadenitis, which is characterized by pyogranulomatous abscess formation. In general, the bacterium causes lesions of the skin, lymph nodes, and internal organs. A disease known as ulcerative lymphagenitis can also result from infection with C. pseudotuberculosis in the distal limbs of horses. This bacterium uses the virulence factors phospholipase D and mycolic acid to damage eukaryotic cell walls and resist phagocytic lysosomal degradation, respectively. Infection with this bacterium is often confirmed by bacterial culture of the purulent exudate. Once the diagnosis has been made, treatment of the infection can begin, but this is difficult due to the nature of the organism and the lesions it forms. Specifically, C. pseudotuberculosis is intrinsically resistant to streptomycin, with varying resistance to penicillin and neomycin depending on the strain. It has been shown to be susceptible to ampicillin, gentamicin, tetracycline, lincomycin, and chloramphenicol. Vaccines have also been produced to develop acquired immunity to this infection.

Abdominal tuberculosis is a type of extrapulmonary tuberculosis which involves the abdominal organs such as intestines, peritoneum and abdominal lymph nodes. It can either occur in isolation or along with a primary focus in patients with disseminated tuberculosis.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Fontanilla JM, Barnes A, von Reyn CF (September 2011). "Current diagnosis and management of peripheral tuberculous lymphadenitis". Clinical Infectious Diseases. 53 (6): 555–562. doi:10.1093/cid/cir454. PMID 21865192.
- ↑ Gopalaswamy R, Dusthackeer VA, Kannayan S, Subbian S (May 26, 2021). "Extrapulmonary Tuberculosis—An Update on the Diagnosis, Treatment and Drug Resistance". Journal of Respiration. 1 (2): 141–164. doi: 10.3390/jor1020015 . ISSN 2673-527X.
- 1 2 Mekonnen D, Derbie A, Abeje A, Shumet A, Nibret E, Biadglegne F, et al. (2019-04-19). "Epidemiology of tuberculous lymphadenitis in Africa: A systematic review and meta-analysis". PLOS ONE. 14 (4): e0215647. Bibcode:2019PLoSO..1415647M. doi: 10.1371/journal.pone.0215647 . PMC 6474617 . PMID 31002716.
- 1 2 Cockerham WC (2016-10-06). International Encyclopedia of Public Health. Academic Press. p. 274. ISBN 9780128037089.
- 1 2 3 4 Bhat SM (2016-06-30). SRB's Manual of Surgery. JP Medical Ltd. pp. 55–56. ISBN 9789351524168.
- ↑ Adigun R, Singh R (2023). "Tuberculosis". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 28722945 . Retrieved 2024-01-06.