Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be no symptoms. Signs and symptoms, when present, may include lower abdominal pain, vaginal discharge, fever, burning with urination, pain with sex, bleeding after sex, or irregular menstruation. Untreated PID can result in long-term complications including infertility, ectopic pregnancy, chronic pelvic pain, and cancer.

Trichomoniasis (trich) is an infectious disease caused by the parasite Trichomonas vaginalis. About 70% of affected people do not have symptoms when infected. When symptoms occur, they typically begin 5 to 28 days after exposure. Symptoms can include itching in the genital area, a bad smelling thin vaginal discharge, burning with urination, and pain with sex. Having trichomoniasis increases the risk of getting HIV/AIDS. It may also cause complications during pregnancy.
Gardnerella vaginalis is a species of Gram-variable-staining facultative anaerobic bacteria. The organisms are small non-spore-forming, nonmotile coccobacilli.
Vaginitis, also known as vulvovaginitis, is inflammation of the vagina and vulva. Symptoms may include itching, burning, pain, discharge, and a bad smell. Certain types of vaginitis may result in complications during pregnancy.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.
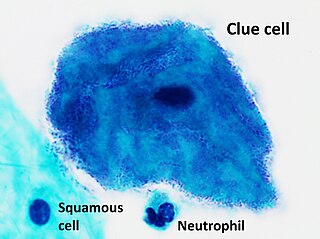
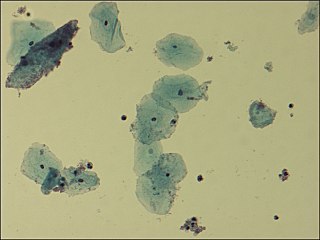
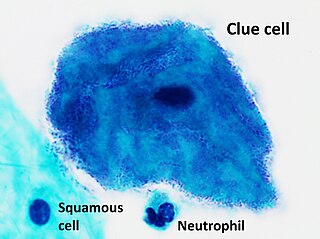
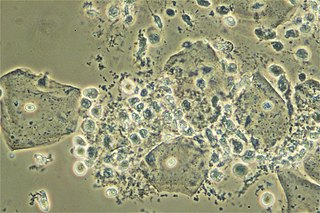
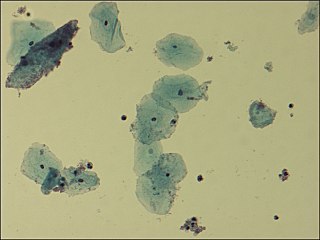
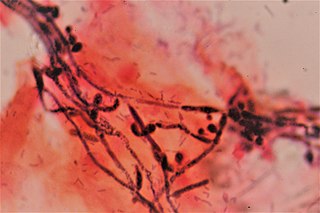
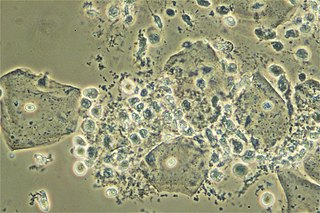
Clue cells are epithelial cells of the vagina that get their distinctive stippled appearance by being covered with bacteria. The etymology behind the term "clue" cell derives from the original research article from Gardner and Dukes describing the characteristic cells. The name was chosen for its brevity in describing the sine qua non of bacterial vaginosis.

Aposymbiosis occurs when symbiotic organisms live apart from one another. Studies have shown that the lifecycles of both the host and the symbiont are affected in some way, usually negative, and that for obligate symbiosis the effects can be drastic. Aposymbiosis is distinct from exsymbiosis, which occurs when organisms are recently separated from a symbiotic association. Because symbionts can be vertically transmitted from parent to offspring or horizontally transmitted from the environment, the presence of an aposymbiotic state suggests that transmission of the symbiont is horizontal. A classical example of a symbiotic relationship with an aposymbiotic state is the Hawaiian bobtail squid Euprymna scolopes and the bioluminescent bacteria Vibrio fischeri. While the nocturnal squid hunts, the bacteria emit light of similar intensity of the moon which camouflages the squid from predators. Juveniles are colonized within hours of hatching and Vibrio must outcompete other bacteria in the seawater through a system of recognition and infection.
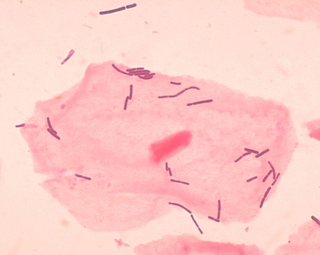
Vaginal flora, vaginal microbiota or vaginal microbiome are the microorganisms that colonize the vagina. They were discovered by the German gynecologist Albert Döderlein in 1892 and are part of the overall human flora. The amount and type of bacteria present have significant implications for an individual's overall health. The primary colonizing bacteria of a healthy individual are of the genus Lactobacillus, such as L. crispatus, and the lactic acid they produce is thought to protect against infection by pathogenic species.
A vaginal disease is a pathological condition that affects part or all of the vagina.
Female genital disease is a disorder of the structure or function of the female reproductive system that has a known cause and a distinctive group of symptoms, signs, or anatomical changes. The female reproductive system consists of the ovaries, fallopian tubes, uterus, vagina, and vulva. Female genital diseases can be classified by affected location or by type of disease, such as malformation, inflammation, or infection.
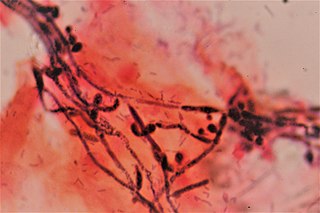
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation. The most common symptom is vaginal itching, which may be severe. Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina. Symptoms often worsen just before a woman's period.
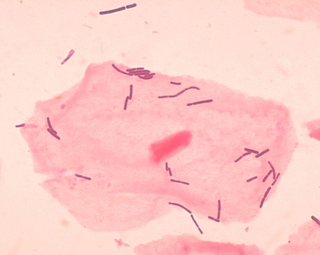
Lactobacillus crispatus is a common, rod-shaped species of genus Lactobacillus and is a hydrogen peroxide (H2O2) producing beneficial microbiota species located in both the vagina, through vaginal discharge, and the vertebrate gastrointestinal tract. The strain CTV-05 is used as a probiotic that can be used by premenopausal and postmenopausal women that experience recurrent urinary tract infections. It is being evaluated specifically for the prevention and treatment of bacterial vaginosis, which is characterized by the absence of Lactobacillus flora necessary to protect the host from infection.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.
Aerobic vaginitis (AV) is a form of vaginitis first described by Donders et al. in 2002. It is characterized by a more or less severe disruption of the lactobacillary flora, along with inflammation, atrophy, and the presence of a predominantly aerobic microflora, composed of enteric commensals or pathogens.

Lactobacillus vaccines are used in the therapy and prophylaxis of non-specific bacterial vaginitis and trichomoniasis. The vaccines consist of specific inactivated strains of Lactobacilli, called "aberrant" strains in the relevant literature dating from the 1980s. These strains were isolated from the vaginal secretions of patients with acute colpitis. The lactobacilli in question are polymorphic, often shortened or coccoid in shape and do not produce an acidic, anti-pathogenic vaginal environment. A colonization with aberrant lactobacilli has been associated with an increased susceptibility to vaginal infections and a high rate of relapse following antimicrobial treatment. Intramuscular administration of inactivated aberrant lactobacilli provokes a humoral immune response. The production of specific antibodies both in serum and in the vaginal secretion has been demonstrated. As a result of the immune stimulation, the abnormal lactobacilli are inhibited, the population of normal, rod-shaped lactobacilli can grow and exert its defense functions against pathogenic microorganisms.
Limosilactobacillus vaginalis is a lactic acid bacterium that is a normal, but infrequent part of the vaginal microbiome.
LACTIN-V, also known as CTV-05 or as Lactobacillus crispatus CTV-05, is a live biopharmaceutical medication containing a strain of Lactobacillus crispatus (L. crispatus) which is under development for the treatment of urinary tract infections (UTIs) and bacterial vaginosis (BV). It is administered intravaginally and is described as the first vaginal microbiome (VMB)-based live biotherapeutic product (LBP). Depletion of hydrogen peroxide (H2O2)-producing Lactobacillus strains such as Lactobacillus crispatus in the vagina has been strongly associated with BV and UTIs. Most commercially available probiotic Lactobacillus strains are not vaginal strains and do not appear to improve vaginal or urinary health outcomes. The Centers for Disease Control and Prevention (CDC)'s Sexually Transmitted Infections Treatment Guidelines (2021) noted that intravaginal LACTIN-V produced a considerably lower recurrence of BV following initial antibiotic treatment with metronidazole in a randomized controlled trial. However, the guidelines also noted that LACTIN-V is not yet Food and Drug Administration (FDA)-approved or commercially available. As of December 2021, LACTIN-V is in phase 2/3 clinical trials for the treatment of UTIs and is in phase 2 trials for the treatment of BV. It was originated by GyneLogix and is under development by Osel Inc., the National Institute of Allergy and Infectious Diseases, and other organizations.

TOL-463 is an anti-infective medication which is under development for the treatment of bacterial vaginosis (BV) and vulvovaginal candidiasis (VVC). It is a boric acid-based vaginal anti-infective enhanced with ethylenediaminetetraacetic acid (EDTA) which was designed to have improved activity against vaginal bacterial and fungal biofilms while sparing protective lactobacilli. EDTA enhances the antimicrobial activity of boric acid and improves its efficacy against relevant biofilms. In a small phase 2 randomized controlled trial, TOL-463 as an insert or gel achieved clinical cure rates of 50–59% against BV and 81–92% against VVC in women who had one or both conditions. It was effective and safe in the study, though it was without indication of superiority over other antifungal medications for VVC. The cure rates against BV with TOL-463 were said to be comparable to those with recently approved antibiotic treatments like single-dose oral secnidazole (58%) and single-dose metronidazole vaginal gel (41%). As of May 2019, TOL-463 is in phase 2 clinical trials for the treatment of BV and VVC. It was originated by Toltec Pharmaceuticals and is under development by Toltec Pharmaceuticals and the National Institute of Allergy and Infectious Diseases.