Related Research Articles

Beta-lactamases, (β-lactamases) are enzymes produced by bacteria that provide multi-resistance to beta-lactam antibiotics such as penicillins, cephalosporins, cephamycins, monobactams and carbapenems (ertapenem), although carbapenems are relatively resistant to beta-lactamase. Beta-lactamase provides antibiotic resistance by breaking the antibiotics' structure. These antibiotics all have a common element in their molecular structure: a four-atom ring known as a beta-lactam (β-lactam) ring. Through hydrolysis, the enzyme lactamase breaks the β-lactam ring open, deactivating the molecule's antibacterial properties.
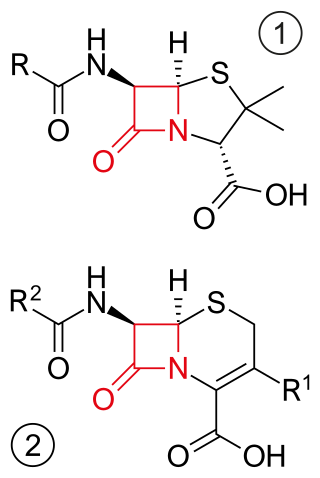
β-lactam antibiotics are antibiotics that contain a beta-lactam ring in their chemical structure. This includes penicillin derivatives (penams), cephalosporins and cephamycins (cephems), monobactams, carbapenems and carbacephems. Most β-lactam antibiotics work by inhibiting cell wall biosynthesis in the bacterial organism and are the most widely used group of antibiotics. Until 2003, when measured by sales, more than half of all commercially available antibiotics in use were β-lactam compounds. The first β-lactam antibiotic discovered, penicillin, was isolated from a strain of Penicillium rubens.

Klebsiella pneumoniae is a Gram-negative, non-motile, encapsulated, lactose-fermenting, facultative anaerobic, rod-shaped bacterium. It appears as a mucoid lactose fermenter on MacConkey agar.

The cephalosporins are a class of β-lactam antibiotics originally derived from the fungus Acremonium, which was previously known as Cephalosporium.

Clavulanic acid is a β-lactam drug that functions as a mechanism-based β-lactamase inhibitor. While not effective by itself as an antibiotic, when combined with penicillin-group antibiotics, it can overcome antibiotic resistance in bacteria that secrete β-lactamase, which otherwise inactivates most penicillins.

Moraxella catarrhalis is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the infection of the host cell by sticking to the host cell using trimeric autotransporter adhesins.

Carbapenems are a class of very effective antibiotic agents most commonly used for the treatment of severe bacterial infections. This class of antibiotics is usually reserved for known or suspected multidrug-resistant (MDR) bacterial infections. Similar to penicillins and cephalosporins, carbapenems are members of the beta lactam class of antibiotics, which kill bacteria by binding to penicillin-binding proteins, thus inhibiting bacterial cell wall synthesis. However, these agents individually exhibit a broader spectrum of activity compared to most cephalosporins and penicillins. Furthermore, carbapenems are typically unaffected by emerging antibiotic resistance, even to other beta-lactams.

Imipenem is an intravenous β-lactam antibiotic discovered by Merck scientists Burton Christensen, William Leanza, and Kenneth Wildonger in the mid-1970s. Carbapenems are highly resistant to the β-lactamase enzymes produced by many multiple drug-resistant Gram-negative bacteria, thus play a key role in the treatment of infections not readily treated with other antibiotics.
Ampicillin/sulbactam is a fixed-dose combination medication of the common penicillin-derived antibiotic ampicillin and sulbactam, an inhibitor of bacterial beta-lactamase. Two different forms of the drug exist. The first, developed in 1987 and marketed in the United States under the brand name Unasyn, generic only outside the United States, is an intravenous antibiotic. The second, an oral form called sultamicillin, is marketed under the brand name Ampictam outside the United States, and generic only in the United States. Ampicillin/sulbactam is used to treat infections caused by bacteria resistant to beta-lactam antibiotics. Sulbactam blocks the enzyme which breaks down ampicillin and thereby allows ampicillin to attack and kill the bacteria.

Sultamicillin, sold under the brand name Unasyn among others, is an oral form of the penicillin antibiotic combination ampicillin/sulbactam. It is used for the treatment of bacterial infections of the upper and lower respiratory tract, the kidneys and urinary tract, skin and soft tissues, among other organs. It contains esterified ampicillin and sulbactam.

Bacteroides fragilis is an anaerobic, Gram-negative, pleomorphic to rod-shaped bacterium. It is part of the normal microbiota of the human colon and is generally commensal, but can cause infection if displaced into the bloodstream or surrounding tissue following surgery, disease, or trauma.
Capnocytophaga canimorsus is a fastidious, slow-growing, Gram-negative rod of the genus Capnocytophaga. It is a commensal bacterium in the normal gingival flora of canine and feline species, but can cause illness in humans. Transmission may occur through bites, licks, or even close proximity with animals. C. canimorsus generally has low virulence in healthy individuals, but has been observed to cause severe, even grave, illness in persons with pre-existing conditions. The pathogenesis of C. canimorsus is still largely unknown, but increased clinical diagnoses have fostered an interest in the bacillus. Treatment with antibiotics is effective in most cases, but the most important yet basic diagnostic tool available to clinicians remains the knowledge of recent exposure to canines or felines.

Acinetobacter baumannii is a typically short, almost round, rod-shaped (coccobacillus) Gram-negative bacterium. It is named after the bacteriologist Paul Baumann. It can be an opportunistic pathogen in humans, affecting people with compromised immune systems, and is becoming increasingly important as a hospital-derived (nosocomial) infection. While other species of the genus Acinetobacter are often found in soil samples, it is almost exclusively isolated from hospital environments. Although occasionally it has been found in environmental soil and water samples, its natural habitat is still not known.

Enterobacter cloacae is a clinically significant Gram-negative, facultatively-anaerobic, rod-shaped bacterium.

Cefoxitin is a second-generation cephamycin antibiotic developed by Merck & Co., Inc. from Cephamycin C in the year following its discovery, 1972. It was synthesized in order to create an antibiotic with a broader spectrum. It is often grouped with the second-generation cephalosporins. Cefoxitin requires a prescription and as of 2010 is sold under the brand name Mefoxin by Bioniche Pharma, LLC. The generic version of cefoxitin is known as cefoxitin sodium.

Beta-lactamases are a family of enzymes involved in bacterial resistance to beta-lactam antibiotics. In bacterial resistance to beta-lactam antibiotics, the bacteria have beta-lactamase which degrade the beta-lactam rings, rendering the antibiotic ineffective. However, with beta-lactamase inhibitors, these enzymes on the bacteria are inhibited, thus allowing the antibiotic to take effect. Strategies for combating this form of resistance have included the development of new beta-lactam antibiotics that are more resistant to cleavage and the development of the class of enzyme inhibitors called beta-lactamase inhibitors. Although β-lactamase inhibitors have little antibiotic activity of their own, they prevent bacterial degradation of beta-lactam antibiotics and thus extend the range of bacteria the drugs are effective against.
Well studied Periodontal pathogens are bacteria that have been shown to significantly contribute to periodontitis.
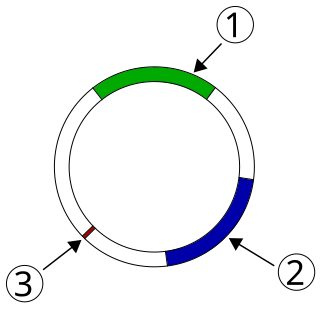
Plasmid-mediated resistance is the transfer of antibiotic resistance genes which are carried on plasmids. Plasmids possess mechanisms that ensure their independent replication as well as those that regulate their replication number and guarantee stable inheritance during cell division. By the conjugation process, they can stimulate lateral transfer between bacteria from various genera and kingdoms. Numerous plasmids contain addiction-inducing systems that are typically based on toxin-antitoxin factors and capable of killing daughter cells that don't inherit the plasmid during cell division. Plasmids often carry multiple antibiotic resistance genes, contributing to the spread of multidrug-resistance (MDR). Antibiotic resistance mediated by MDR plasmids severely limits the treatment options for the infections caused by Gram-negative bacteria, especially family Enterobacteriaceae. The global spread of MDR plasmids has been enhanced by selective pressure from antimicrobial medications used in medical facilities and when raising animals for food.
Anaerobic infections are caused by anaerobic bacteria. Obligately anaerobic bacteria do not grow on solid media in room air ; facultatively anaerobic bacteria can grow in the presence or absence of air. Microaerophilic bacteria do not grow at all aerobically or grow poorly, but grow better under 10% carbon dioxide or anaerobically. Anaerobic bacteria can be divided into strict anaerobes that can not grow in the presence of more than 0.5% oxygen and moderate anaerobic bacteria that are able of growing between 2 and 8% oxygen. Anaerobic bacteria usually do not possess catalase, but some can generate superoxide dismutase which protects them from oxygen.

Neisseria gonorrhoeae, the bacterium that causes the sexually transmitted infection gonorrhea, has developed antibiotic resistance to many antibiotics. The bacteria was first identified in 1879.
References
- 1 2 3 Parte, A.C. "Capnocytophaga". LPSN .
- ↑ Jolivet-Gougeon A, Sixou JL, Tamanai-Shacoori Z, Bonnaure-Mallet M (April 2007). "Antimicrobial treatment of Capnocytophaga infections". International Journal of Antimicrobial Agents. 29 (4): 367–73. doi:10.1016/j.ijantimicag.2006.10.005. PMID 17250994.
- ↑ Ehrmann E, Jolivet-Gougeon A, Bonnaure-Mallet M, Fosse T (October 2013). "Antibiotic content of selective culture media for isolation of Capnocytophaga species from oral polymicrobial samples". Letters in Applied Microbiology. 57 (4): 303–9. doi:10.1111/lam.12112. PMID 23725093. S2CID 206168867.
- 1 2 3 Guillon H, Eb F, Mammeri H (May 2010). "Characterization of CSP-1, a novel extended-spectrum beta-lactamase produced by a clinical isolate of Capnocytophaga sputigena". Antimicrobial Agents and Chemotherapy. 54 (5): 2231–4. doi:10.1128/AAC.00791-09. PMC 2863690 . PMID 20308380.
- ↑ McGuire, Michael K.; Nunn, Martha E. (1996). "Prognosis Versus Actual Outcome. III. The Effectiveness of Clinical Parameters in Accurately Predicting Tooth Survival". Journal of Periodontology. 67 (7): 666–674. doi:10.1902/jop.1996.67.7.666. PMID 8832477.
- ↑ Jolivet-Gougeon A, Guérin J, Tamanai-Shacoori Z, Gandemer V, Sixou JL, Bonnaure-Mallet M (July 2008). "Influence of previous antimicrobial therapy on oral carriage of beta-lactamase producing Capnocytophaga isolates". Acta Paediatrica. Oslo, Norway. 97 (7): 964–7. doi:10.1111/j.1651-2227.2008.00824.x. PMID 18532936. S2CID 12600819.
- ↑ Sixou JL, Aubry-Leuliette A, De Medeiros-Battista O, Lejeune S, Jolivet-Gougeon A, Solhi-Pinsard H, Gandemer V, Barbosa-Rogier M, Bonnaure-Mallet M (March 2006). "Capnocytophaga in the dental plaque of immunocompromised children with cancer". International Journal of Paediatric Dentistry. 16 (2): 75–80. doi:10.1111/j.1365-263X.2006.00697.x. PMID 16430520.
- ↑ Ma A, Goetz MB (January 2013). "Capnocytophaga canimorsus sepsis with associated thrombotic thrombocytopenic purpura". The American Journal of the Medical Sciences. 345 (1): 78–80. doi:10.1097/MAJ.0b013e318262db1a. PMID 22990045.
- 1 2 3 Jolivet-Gougeon A, Sixou JL, Tamanai-Shacoori Z, Bonnaure-Mallet M (April 2007). "Antimicrobial treatment of Capnocytophaga infections". International Journal of Antimicrobial Agents. 29 (4): 367–73. doi:10.1016/j.ijantimicag.2006.10.005. PMID 17250994.
- 1 2 3 Jolivet-Gougeon A, Tamanai-Shacoori Z, Desbordes L, Burggraeve N, Cormier M, Bonnaure-Mallet M (February 2004). "Genetic analysis of an ambler class A extended-spectrum beta-lactamase from Capnocytophaga ochracea". Journal of Clinical Microbiology. 42 (2): 888–90. doi:10.1128/jcm.42.2.888-890.2004. PMC 344468 . PMID 14766881.
- ↑ Handal T, Olsen I, Walker CB, Caugant DA (January 2005). "Detection and characterization of beta-lactamase genes in subgingival bacteria from patients with refractory periodontitis". FEMS Microbiology Letters. 242 (2): 319–24. doi: 10.1016/j.femsle.2004.11.023 . PMID 15621454.
- ↑ Rogers MB, Parker AC, Smith CJ (November 1993). "Cloning and characterization of the endogenous cephalosporinase gene, cepA, from Bacteroides fragilis reveals a new subgroup of Ambler class A beta-lactamases". Antimicrobial Agents and Chemotherapy. 37 (11): 2391–400. doi:10.1128/aac.37.11.2391. PMC 192397 . PMID 8285623.
- ↑ Piau C, Arvieux C, Bonnaure-Mallet M, Jolivet-Gougeon A (June 2013). "Capnocytophaga spp. involvement in bone infections: a review". International Journal of Antimicrobial Agents. 41 (6): 509–15. doi:10.1016/j.ijantimicag.2013.03.001. PMID 23642766.
- ↑ Lion C, Escande F, Burdin JC (October 1996). "Capnocytophaga canimorsus infections in human: review of the literature and cases report". European Journal of Epidemiology. 12 (5): 521–33. doi:10.1007/BF00144007. PMID 8905316. S2CID 22408402.