Gram-negative bacteria are bacteria that do not retain the crystal violet stain used in the Gram staining method of bacterial differentiation. Their defining characteristic is their cell envelopes, which consists of a thin peptidoglycan cell wall sandwiched between an inner (cytoplasmic) membrane and an outer membrane. These bacteria are found in all environments that support life on Earth.

Streptococcus is a genus of gram-positive coccus or spherical bacteria that belongs to the family Streptococcaceae, within the order Lactobacillales, in the phylum Bacillota. Cell division in streptococci occurs along a single axis, so as they grow, they tend to form pairs or chains that may appear bent or twisted. This differs from staphylococci, which divide along multiple axes, thereby generating irregular, grape-like clusters of cells. Most streptococci are oxidase-negative and catalase-negative, and many are facultative anaerobes.

Neisseria gonorrhoeae, also known as gonococcus (singular) or gonococci (plural), is a species of Gram-negative diplococci bacteria isolated by Albert Neisser in 1879. It causes the sexually transmitted genitourinary infection gonorrhea as well as other forms of gonococcal disease including disseminated gonococcemia, septic arthritis, and gonococcal ophthalmia neonatorum.

Waterhouse–Friderichsen syndrome (WFS) is defined as adrenal gland failure due to bleeding into the adrenal glands, commonly caused by severe bacterial infection. Typically, it is caused by Neisseria meningitidis.
Bloodstream infections (BSIs) are infections of blood caused by blood-borne pathogens. Blood is normally a sterile environment, so the detection of microbes in the blood is always abnormal. A bloodstream infection is different from sepsis, which is characterized by severe inflammatory or immune responses of the host organism to pathogens.

Listeria monocytogenes is the species of pathogenic bacteria that causes the infection listeriosis. It is a facultative anaerobic bacterium, capable of surviving in the presence or absence of oxygen. It can grow and reproduce inside the host's cells and is one of the most virulent foodborne pathogens: 20 to 30% of foodborne listeriosis infections in high-risk individuals may be fatal. In the European Union, listeriosis follows an upward trend that began in 2008, causing 2,161 confirmed cases and 210 reported deaths in 2014, 16% more than in 2013. Listeriosis mortality rates are also higher in the EU than for other foodborne pathogens. Responsible for an estimated 1,600 illnesses and 260 deaths in the United States annually, listeriosis ranks third in total number of deaths among foodborne bacterial pathogens, with fatality rates exceeding even Salmonella spp. and Clostridium botulinum.
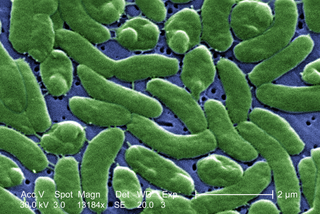
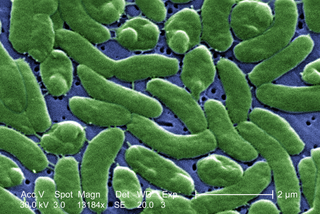
Vibrio vulnificus is a species of Gram-negative, motile, curved rod-shaped (vibrio), pathogenic bacteria of the genus Vibrio. Present in marine environments such as estuaries, brackish ponds, or coastal areas, V. vulnificus is related to V. cholerae, the causative agent of cholera. At least one strain of V. vulnificus is bioluminescent. Increasing seasonal ocean temperatures and low-salt marine environments like estuaries favor a greater concentration of Vibrio within filter-feeding shellfish; V. vulnificus infections in the Eastern United States have increased eightfold from 1988–2018.

Haemophilus influenzae is a Gram-negative, non-motile, coccobacillary, facultatively anaerobic, capnophilic pathogenic bacterium of the family Pasteurellaceae. The bacteria are mesophilic and grow best at temperatures between 35 and 37 °C.
An overwhelming post-splenectomy infection (OPSI) is a rare but rapidly fatal infection occurring in individuals following removal of the spleen. The infections are typically characterized by either meningitis or sepsis, and are caused by encapsulated organisms including Streptococcus pneumoniae. It is a medical emergency and requires immediate treatment. Death has been reported to occur within 12 hours.

Neisseria meningitidis, often referred to as the meningococcus, is a Gram-negative bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia, a life-threatening sepsis. The bacterium is referred to as a coccus because it is round, and more specifically a diplococcus because of its tendency to form pairs.

Moraxella catarrhalis is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the infection of the host cell by sticking to the host cell using trimeric autotransporter adhesins.

Meningococcal disease describes infections caused by the bacterium Neisseria meningitidis. It has a high mortality rate if untreated but is vaccine-preventable. While best known as a cause of meningitis, it can also result in sepsis, which is an even more damaging and dangerous condition. Meningitis and meningococcemia are major causes of illness, death, and disability in both developed and under-developed countries.

Eikenella corrodens is a Gram-negative facultative anaerobic bacillus that can cause severe invasive disease in humans. It was first identified by M. Eiken in 1958, who called it Bacteroides corrodens. E. corrodens is a rare pericarditis associated pathogen. It is a fastidious, slow growing, human commensal bacillus, capable of acting as an opportunistic pathogen and causing abscesses in several anatomical sites, including the liver, lung, spleen, and submandibular region. E. corrodens could independently cause serious infection in both immunocompetent and immunocompromised hosts.

Elizabethkingia meningoseptica is a Gram-negative, rod-shaped bacterium widely distributed in nature. It may be normally present in fish and frogs; it may be isolated from chronic infectious states, as in the sputum of cystic fibrosis patients. In 1959, American bacteriologist Elizabeth O. King was studying unclassified bacteria associated with pediatric meningitis at the Centers for Disease Control and Prevention in Atlanta, when she isolated an organism that she named Flavobacterium meningosepticum. In 1994, it was reclassified in the genus Chryseobacterium and renamed Chryseobacterium meningosepticum(chryseos = "golden" in Greek, so Chryseobacterium means a golden/yellow rod similar to Flavobacterium). In 2005, a 16S rRNA phylogenetic tree of Chryseobacteria showed that C. meningosepticum along with C. miricola were close to each other but outside the tree of the rest of the Chryseobacteria and were then placed in a new genus Elizabethkingia named after the original discoverer of F. meningosepticum.

Ehrlichiosis is a tick-borne bacterial infection, caused by bacteria of the family Anaplasmataceae, genera Ehrlichia and Anaplasma. These obligate intracellular bacteria infect and kill white blood cells.
Pseudomonas oryzihabitans is a nonfermenting yellow-pigmented, gram-negative, rod-shaped bacterium that can cause sepsis, peritonitis, endophthalmitis, and bacteremia. It is an opportunistic pathogen of humans and warm-blooded animals that is commonly found in several environmental sources, from soil to rice paddies. They can be distinguished from other nonfermenters by their negative oxidase reaction and aerobic character. This organism can infect individuals that have major illnesses, including those undergoing surgery or with catheters in their body. Based on the 16S RNA analysis, these bacteria have been placed in the Pseudomonas putida group.
Capnocytophaga is a genus of Gram-negative bacteria. Normally found in the oropharyngeal tract of mammals, they are involved in the pathogenesis of some animal bite wounds and periodontal diseases.

Pathogenic bacteria are bacteria that can cause disease. This article focuses on the bacteria that are pathogenic to humans. Most species of bacteria are harmless and are often beneficial but others can cause infectious diseases. The number of these pathogenic species in humans is estimated to be fewer than a hundred. By contrast, several thousand species are part of the gut flora present in the digestive tract.
Citrobacter koseri, formerly known as Citrobacter diversus, is a Gram-negative non-spore forming, rod-shaped bacterium. It is a facultative anaerobe capable of aerobic respiration. It is motile via peritrichous flagella. It is a member of the family of Enterobacteriaceae. The members of this family are part of the normal flora and commonly found in the digestive tracts of humans and animals. C. koseri may act as an opportunistic pathogen in individuals who are immunocompromised.

A feline zoonosis is a viral, bacterial, fungal, protozoan, nematode or arthropod infection that can be transmitted to humans from the domesticated cat, Felis catus. Some of these diseases are reemerging and newly emerging infections or infestations caused by zoonotic pathogens transmitted by cats. In some instances, the cat can display symptoms of infection and sometimes the cat remains asymptomatic. There can be serious illnesses and clinical manifestations in people who become infected. This is dependent on the immune status and age of the person. Those who live in close association with cats are more prone to these infections, but those that do not keep cats as pets can also acquire these infections as the transmission can be from cat feces and the parasites that leave their bodies.