Lyme disease, also known as Lyme borreliosis, is a tick-borne disease caused by species of Borrelia bacteria, transmitted by blood-feeding ticks in the genus Ixodes. The most common sign of infection is an expanding red rash, known as erythema migrans (EM), which appears at the site of the tick bite about a week afterwards. The rash is typically neither itchy nor painful. Approximately 70–80% of infected people develop a rash. Early diagnosis can be difficult. Other early symptoms may include fever, headaches and tiredness. If untreated, symptoms may include loss of the ability to move one or both sides of the face, joint pains, severe headaches with neck stiffness or heart palpitations. Months to years later, repeated episodes of joint pain and swelling may occur. Occasionally, shooting pains or tingling in the arms and legs may develop. Despite appropriate treatment, about 10 to 20% of those affected develop joint pains, memory problems, and tiredness for at least six months.

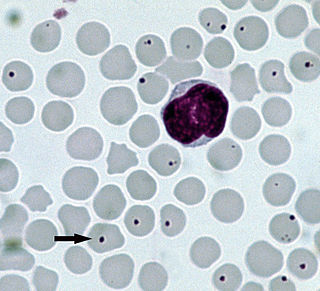
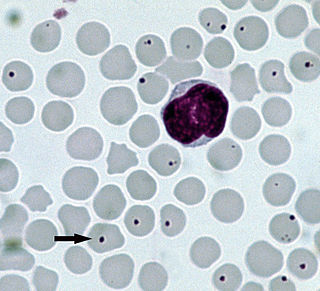
Babesiosis or piroplasmosis is a malaria-like parasitic disease caused by infection with a eukaryotic parasite in the order Piroplasmida, typically a Babesia or Theileria, in the phylum Apicomplexa. Human babesiosis transmission via tick bite is most common in the Northeastern and Midwestern United States and parts of Europe, and sporadic throughout the rest of the world. It occurs in warm weather. People can get infected with Babesia parasites by the bite of an infected tick, by getting a blood transfusion from an infected donor of blood products, or by congenital transmission . Ticks transmit the human strain of babesiosis, so it often presents with other tick-borne illnesses such as Lyme disease. After trypanosomes, Babesia is thought to be the second-most common blood parasite of mammals. They can have major adverse effects on the health of domestic animals in areas without severe winters. In cattle, the disease is known as Texas cattle fever or redwater.

A rash is a change of the skin that affects its color, appearance, or texture.
Tick-borne diseases, which afflict humans and other animals, are caused by infectious agents transmitted by tick bites. They are caused by infection with a variety of pathogens, including rickettsia and other types of bacteria, viruses, and protozoa. The economic impact of tick-borne diseases is considered to be substantial in humans, and tick-borne diseases are estimated to affect ~80 % of cattle worldwide. Most of these pathogens require passage through vertebrate hosts as part of their life cycle. Tick-borne infections in humans, farm animals, and companion animals are primarily associated with wildlife animal reservoirs. Many tick-borne infections in humans involve a complex cycle between wildlife animal reservoirs and tick vectors. The survival and transmission of these tick-borne viruses are closely linked to their interactions with tick vectors and host cells. These viruses are classified into different families, including Asfarviridae, Reoviridae, Rhabdoviridae, Orthomyxoviridae, Bunyaviridae, and Flaviviridae.

Borrelia burgdorferi is a bacterial species of the spirochete class in the genus Borrelia, and is one of the causative agents of Lyme disease in humans. Along with a few similar genospecies, some of which also cause Lyme disease, it makes up the species complex of Borrelia burgdorferi sensu lato. The complex currently comprises 20 accepted and 3 proposed genospecies. B. burgdorferi sensu stricto exists in North America and Eurasia and until 2016 was the only known cause of Lyme disease in North America. Borrelia species are Gram-negative.
Rat-bite fever (RBF) is an acute, febrile human illness caused by bacteria transmitted by rodents, in most cases, which is passed from rodent to human by the rodent's urine or mucous secretions. Alternative names for rat-bite fever include streptobacillary fever, streptobacillosis, spirillary fever, bogger, and epidemic arthritic erythema. It is a rare disease spread by infected rodents and caused by two specific types of bacteria:
- Streptobacillus moniliformis, the only reported bacteria that causes RBF in North America
- Spirillum minus, common in Asia. Most cases occur in Japan, but specific strains of the disease are present in the United States, Europe, Australia, and Africa.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Anaplasmosis is a tick-borne disease affecting ruminants, dogs, and horses, and is caused by Anaplasma bacteria. Anaplasmosis is an infectious but not contagious disease. Anaplasmosis can be transmitted through mechanical and biological vector processes. Anaplasmosis can also be referred to as "yellow bag" or "yellow fever" because the infected animal can develop a jaundiced look. Other signs of infection include weight loss, diarrhea, paleness of the skin, aggressive behavior, and high fever.
Jorge Benach is a medical researcher at the Stony Brook University in New York state. Benach is the chair of the Department of Molecular Genetics and Microbiology. Benach's main area of research is the tick-borne spirochete Borrelia burgdorferi, which is the causative agent of Lyme disease.
Allen Caruthers Steere is an American rheumatologist. He is a professor of rheumatology at Harvard University and previously at Tufts University and Yale University. Steere and his mentor, Stephen Malawista of Yale University, are credited with discovering and naming Lyme disease, and he has published almost 300 scholarly articles on Lyme disease during his more than 40 years of studies of this infection. At a ceremony in Hartford, Connecticut in 1998, Governor John G. Rowland declared September 24 to be "Allen C. Steere Day".
Neuroborreliosis is a disorder of the central nervous system. A neurological manifestation of Lyme disease, neuroborreliosis is caused by a systemic infection of spirochetes of the genus Borrelia. Symptoms of the disease include erythema migrans and flu-like symptoms.

Southern tick-associated rash illness (STARI) is an emerging infectious disease related to Lyme disease that occurs in southeastern and south-central United States. It is spread by tick bites and it was hypothesized that the illness was caused by the bacteria Borrelia lonestari. However, there is insufficient evidence to declare this Borrelia strain as a causative agent.

Human granulocytic anaplasmosis (HGA) is a tick-borne, infectious disease caused by Anaplasma phagocytophilum, an obligate intracellular bacterium that is typically transmitted to humans by ticks of the Ixodes ricinus species complex, including Ixodes scapularis and Ixodes pacificus in North America. These ticks also transmit Lyme disease and other tick-borne diseases.
The International Lyme and Associated Diseases Society is a non-profit advocacy group which advocates for greater acceptance of the controversial and unrecognized diagnosis "chronic Lyme disease". ILADS was formed by advocates for the recognition of "chronic Lyme disease" including physicians, patients and laboratory personnel, and has published alternative treatment guidelines and diagnostic criteria due to the disagreement with mainstream consensus medical views on Lyme disease.
In dermatology, a target lesion or bull's-eye lesion, named for its resemblance to the bull's-eye of a shooting target, is a rash with central clearing. It occurs in several diseases, as follows:
Rickettsia helvetica, previously known as the Swiss agent, is a bacterium found in Dermacentor reticulatus and other ticks, which has been implicated as a suspected but unconfirmed human pathogen. First recognized in 1979 in Ixodes ricinus ticks in Switzerland as a new member of the spotted fever group of Rickettsia, the R. helvetica bacterium was eventually isolated in 1993. Although R. helvetica was initially thought to be harmless in humans and many animal species, some individual case reports suggest that it may be capable of causing a nonspecific fever in humans. In 1997, a man living in eastern France seroconverted to Rickettsia 4 weeks after onset of an unexplained febrile illness. In 2010, a case report indicated that tick-borne R. helvetica can also cause meningitis in humans.
Borrelia miyamotoi is a bacterium of the spirochete phylum in the genus Borrelia. A zoonotic organism, B. miyamotoi can infect humans through the bite of several species of hard-shell Ixodes ticks, the same kind of ticks that spread B. burgdorferi, the causative bacterium of Lyme disease. Ixodes ticks are also the primary vector in the spread of babesiosis and anaplasmosis.
Chronic Lyme disease (CLD) is the name used by some people with non-specific symptoms, such as fatigue, muscle pain, and cognitive dysfunction to refer to their condition, even if there is no evidence that they had Lyme disease. Both the label and the belief that these people's symptoms are caused by this particular infection are generally rejected by medical professionals. Chronic Lyme disease is distinct from post-treatment Lyme disease syndrome, a set of lingering symptoms which may persist after successful antibiotic treatment of infection with Lyme-causing Borrelia bacteria, and which may have similar symptoms to those associated with CLD.

The Baggio–Yoshinari syndrome, formerly known as the Brazilian Lyme-like disease and Brazilian human borreliosis, is a disease transmitted by the Amblyomma cajennense tick, but the organism that causes the infection is still unknown. Clinical features resemble those of Lyme disease (LD).
Lymphocytic meningoradiculitis, also known as Bannwarth syndrome, is a neurological disease characterized as intense nerve pain radiating from the spine. The disease is caused by an infection of Borrelia burgdorferi, a tick-borne spirochete bacterium also responsible for causing Lyme disease.