Dermatitis is inflammation of the skin, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened. The area of skin involved can vary from small to covering the entire body. Dermatitis is often called eczema, and the difference between those terms is not standardized.

Acne, also known as acne vulgaris, is a long-term skin condition that occurs when dead skin cells and oil from the skin clog hair follicles. Typical features of the condition include blackheads or whiteheads, pimples, oily skin, and possible scarring. It primarily affects skin with a relatively high number of oil glands, including the face, upper part of the chest, and back. The resulting appearance can lead to lack of confidence, anxiety, reduced self-esteem, and, in extreme cases, depression or thoughts of suicide.

Dandruff is a skin condition that mainly affects the scalp. Symptoms include flaking and sometimes mild itchiness. It can result in social or self-esteem problems. A more severe form of the condition, which includes inflammation of the skin, is known as seborrhoeic dermatitis.

Tinea versicolor is a condition characterized by a skin eruption on the trunk and proximal extremities. The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfur is responsible for a small number of cases. These yeasts are normally found on the human skin and become troublesome only under certain conditions, such as a warm and humid environment, although the exact conditions that cause initiation of the disease process are poorly understood.

A sebaceous gland or oil gland is a microscopic exocrine gland in the skin that opens into a hair follicle to secrete an oily or waxy matter, called sebum, which lubricates the hair and skin of mammals. In humans, sebaceous glands occur in the greatest number on the face and scalp, but also on all parts of the skin except the palms of the hands and soles of the feet. In the eyelids, meibomian glands, also called tarsal glands, are a type of sebaceous gland that secrete a special type of sebum into tears. Surrounding the female nipple, areolar glands are specialized sebaceous glands for lubricating the nipple. Fordyce spots are benign, visible, sebaceous glands found usually on the lips, gums and inner cheeks, and genitals.

Zinc pyrithione is a coordination complex of zinc. It has fungistatic and bacteriostatic properties and is used in the treatment of seborrhoeic dermatitis and dandruff.

Ketoconazole, sold under the brand name Nizoral among others, is an antiandrogen, antifungal, and antiglucocorticoid medication used to treat a number of fungal infections. Applied to the skin it is used for fungal skin infections such as tinea, cutaneous candidiasis, pityriasis versicolor, dandruff, and seborrheic dermatitis. Taken by mouth it is a less preferred option and only recommended for severe infections when other agents cannot be used. Other uses include treatment of excessive male-patterned hair growth in women and Cushing's syndrome.

Tinea capitis is a cutaneous fungal infection (dermatophytosis) of the scalp. The disease is primarily caused by dermatophytes in the genera Trichophyton and Microsporum that invade the hair shaft. The clinical presentation is typically single or multiple patches of hair loss, sometimes with a 'black dot' pattern, that may be accompanied by inflammation, scaling, pustules, and itching. Uncommon in adults, tinea capitis is predominantly seen in pre-pubertal children, more often boys than girls.
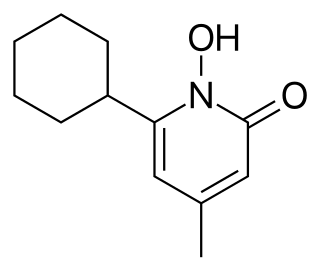
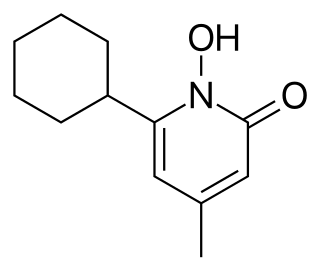
Ciclopirox is a synthetic antifungal agent for topical dermatologic treatment of superficial mycoses. It is most useful against tinea versicolor. It is often used clinically as ciclopirox olamine, the olamine salt of ciclopirox.
The management of hair loss, includes prevention and treatment of alopecia, baldness, and hair thinning, and regrowth of hair.

Cradle cap causes crusty or oily scaly patches on a baby's scalp. The condition is not painful or itchy, but it can cause thick white or yellow scales that are not easy to remove. Cradle cap most commonly begins sometime in the first three months but can occur in later years. Similar symptoms in older children are more likely to be dandruff than cradle cap. The rash is often prominent around the ear, the eyebrows or the eyelids. It may appear in other locations as well, where it is called infantile seborrhoeic dermatitis. Cradle cap is just a special—and more benign—case of this condition. The exact cause of cradle cap is not known. Cradle cap is not spread from person to person (contagious). It is also not caused by poor hygiene. It is not an allergy, and it is not dangerous. Cradle cap often lasts a few months. In some children, the condition can last until age 2 or 3.
Selenium disulfide, also known as selenium sulfide, is a chemical compound and medication used to treat seborrheic dermatitis, dandruff, and pityriasis versicolor. It is applied to the affected area as a lotion or shampoo. Symptoms frequently return if treatment is stopped.

Malassezia furfur is a species of yeast that is naturally found on the skin surfaces of humans and some other mammals. It is associated with a variety of dermatological conditions caused by fungal infections, notably seborrhoeic dermatitis and tinea versicolor. As an opportunistic pathogen, it has further been associated with dandruff, malassezia folliculitis, pityriasis versicolor (alba), and malassezia intertrigo, as well as catheter-related fungemia and pneumonia in patients receiving hematopoietic transplants.

Neonatal acne, also known as acne neonatorum, is a type of acne that develops in newborns, typically before 6 weeks of life. It presents with open and closed comedones on the cheeks, chin and forehead.

Pityriasis amiantacea is an eczematous condition of the scalp in which thick tenaciously adherent scale infiltrates and surrounds the base of a group of scalp hairs. It does not result in scarring or alopecia.

Climbazole is a topical antifungal agent commonly used in the treatment of human fungal skin infections such as dandruff, seborrhoeic dermatitis and eczema. Climbazole has shown a high in vitro and in vivo efficacy against Malassezia spp. that appear to play an important role in the pathogenesis of dandruff. Its chemical structure and properties are similar to other azole fungicides such as ketoconazole, clotrimazole and miconazole.
Anti-seborrheics are drugs effective in seborrheic dermatitis. Selenium sulfide, zinc pyrithione, corticosteroids, imidazole antifungals, and salicylic acid are common anti-seborrheics.
Malassezia sympodialis is a species in the genus Malassezia. It is characterized by a pronounced lipophily, unilateral, percurrent or sympodial budding and an irregular, corrugated cell wall ultrastructure. It is one of the most common species found on the skin of healthy and diseased individuals. It is considered to be part of the skin's normal human microbiota and begins to colonize the skin of humans shortly after birth. Malassezia sympodialis, often has a symbiotic or commensal relationship with its host, but it can act as a pathogen causing a number of different skin diseases, such as atopic dermatitis.

Pyrithione is the common name of an organosulfur compound with molecular formula C
5H
5NOS, chosen as an abbreviation of pyridinethione, and found in the Persian shallot. It exists as a pair of tautomers, the major form being the thione 1-hydroxy-2(1H)-pyridinethione and the minor form being the thiol 2-mercaptopyridine N-oxide; it crystallises in the thione form. It is usually prepared from either 2-bromopyridine, 2-chloropyridine, or 2-chloropyridine N-oxide, and is commercially available as both the neutral compound and its sodium salt. It is used to prepare zinc pyrithione, which is used primarily to treat dandruff and seborrhoeic dermatitis in medicated shampoos, though is also an anti-fouling agent in paints.
Topical antifungaldrugs are used to treat fungal infections on the skin, scalp, nails, vagina or inside the mouth. These medications come as creams, gels, lotions, ointments, powders, shampoos, tinctures and sprays. Most antifungal drugs induce fungal cell death by destroying the cell wall of the fungus. These drugs inhibit the production of ergosterol, which is a fundamental component of the fungal cell membrane and wall.