Dermatitis is inflammation of the skin, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened. The area of skin involved can vary from small to covering the entire body. Dermatitis is often called eczema, and the difference between those terms is not standardized.

A sebaceous gland or oil gland is a microscopic exocrine gland in the skin that opens into a hair follicle to secrete an oily or waxy matter, called sebum, which lubricates the hair and skin of mammals. In humans, sebaceous glands occur in the greatest number on the face and scalp, but also on all parts of the skin except the palms of the hands and soles of the feet. In the eyelids, meibomian glands, also called tarsal glands, are a type of sebaceous gland that secrete a special type of sebum into tears. Surrounding the female nipple, areolar glands are specialized sebaceous glands for lubricating the nipple. Fordyce spots are benign, visible, sebaceous glands found usually on the lips, gums and inner cheeks, and genitals.

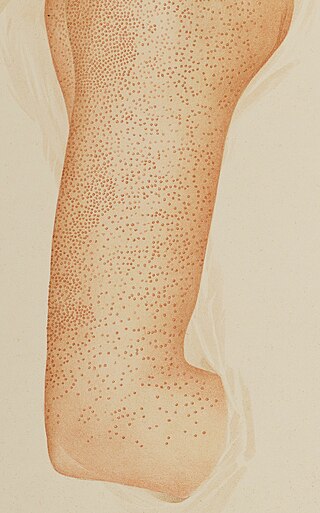
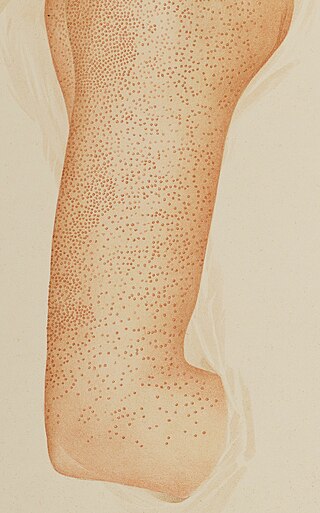
Ichthyosis vulgaris is a skin disorder causing dry, scaly skin. It is the most common form, and one of the mildest forms, of ichthyosis, affecting around 1 in 250 people. For this reason it is known as common ichthyosis. It is usually an autosomal dominant inherited disease, although a rare non-heritable version called acquired ichthyosis exists.
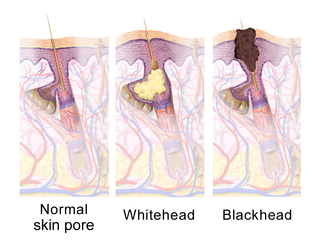
Hyperkeratinization is a disorder of the cells lining the inside of a hair follicle. It is the normal function of these cells to detach or slough off from the skin lining at normal intervals. The dead cells are then forced out of the follicle. However, in hyperkeratinization, this process is interrupted and a number of these dead skin cells do not leave the follicle because of an excess of keratin, a natural protein found in the skin. This excess of keratin, which is influenced by genetics, results in an increased adherence/bonding of dead skin cells together. This cohesion of cells will block or "cap" the hair follicle or clog the sebaceous/oil duct. Pathogens may also play a role in causing, perpetuating, or simply taking advantage of this phenomenon, such as virulent sub-strains of Cutibacterium acnes and irregular migration of Staphylococcus epidermidis from the outer surface of the skin into the follicle, where commensal strains of C. acnes exclusively habitate. It itches mildly at times, and strongly at others. Very often it cannot be felt at all.

Pseudofolliculitis barbae (PFB) is a type of irritant folliculitis that commonly affects people who have curly or coarse facial hair. It occurs when hair curls back into the skin after shaving, causing inflammation, redness, and bumps. This can lead to ingrown hairs, scarring, and skin discoloration. PFB can be treated with various methods, including changing shaving habits, using topical creams or ointments, and undergoing laser hair removal. Prevention measures include proper shaving techniques, using sharp razors, and avoiding too close a shave.

Hyperkeratosis is thickening of the stratum corneum, often associated with the presence of an abnormal quantity of keratin, and is usually accompanied by an increase in the granular layer. As the corneum layer normally varies greatly in thickness in different sites, some experience is needed to assess minor degrees of hyperkeratosis.
Pityriasis rubra pilaris refers to a group of chronic disorders characterized by reddish orange, scaling plaques and keratotic follicular papules. Symptoms may include reddish-orange patches on the skin, severe flaking, uncomfortable itching, thickening of the skin on the feet and hands, and thickened bumps around hair follicles. For some, early symptoms may also include generalized swelling of the legs, feet and other parts of the body. PRP has a varied clinical progression and a varied rate of improvement. There is currently no known cause or cure for PRP.
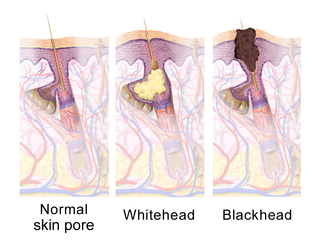
A comedo is a clogged hair follicle (pore) in the skin. Keratin combines with oil to block the follicle. A comedo can be open (blackhead) or closed by skin (whitehead) and occur with or without acne. The word "comedo" comes from the Latin comedere, meaning "to eat up", and was historically used to describe parasitic worms; in modern medical terminology, it is used to suggest the worm-like appearance of the expressed material.

Erythroderma is an inflammatory skin disease with redness and scaling that affects nearly the entire cutaneous surface. This term applies when 90% or more of the skin is affected.

Perioral dermatitis, also known as periorificial dermatitis, is a common type of skin rash. Symptoms include multiple small (1–2 mm) bumps and blisters sometimes with background redness and scale, localized to the skin around the mouth and nostrils. Less commonly the eyes and genitalia may be involved. It can be persistent or recurring and resembles particularly rosacea and to some extent acne and allergic dermatitis. The term "dermatitis" is a misnomer because this is not an eczematous process.
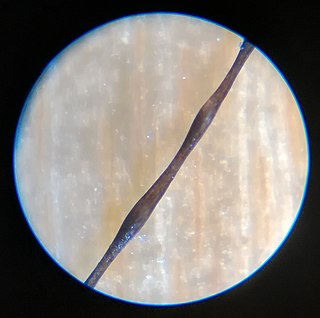
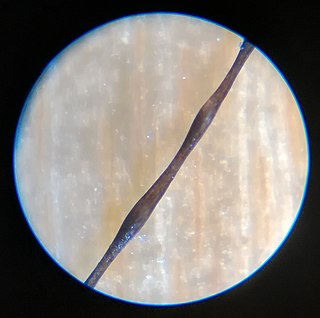
Monilethrix is a rare autosomal dominant hair disease that results in short, fragile, broken hair that appears beaded. It comes from the Latin word for necklace (monile) and the Greek word for hair (thrix). Hair becomes brittle, and breaks off at the thinner parts between the beads. It appears as a thinning or baldness of hair and was first described in 1897 by Walter Smith

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, painful, inflamed and coin-shaped patches of skin with a scaly and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.
Madarosis is a condition that results in the loss of eyelashes, and sometimes eyebrows. The term "madarosis" is derived from the ancient Greek "madaros", meaning "bald". It originally was a disease of only losing eyelashes but it currently is the loss of both eyelashes and eyebrows. Eyebrows and eyelashes are both important in the prevention of bacteria and other foreign objects from entering the eye. A majority of patients with madarosis have leprosy, and it was reported that 76% of patients with varying types of leprosy had madarosis.
Pruritic folliculitis of pregnancy is a skin condition that occurs in one in 3000 people, about 0.2% of cases, who are in their second to third trimester of pregnancy where the hair follicle becomes inflamed or infected, resulting in a pus filled bump. Some dermatologic conditions aside from pruritic folliculitis during pregnancy include "pruritic urticarial papules and plaques of pregnancy, atopic eruption of pregnancy, pemphigoid gestationis, intrahepatic cholestasis of pregnancy, and pustular psoriasis of pregnancy". This pruritic folliculitis of pregnancy differs from typical pruritic folliculitis; in pregnancy, it is characterized by sterile hair follicles becoming inflamed mainly involving the trunk, contrasting how typical pruritic folliculitis is mainly localized on "the upper back, shoulders, and chest." This condition was first observed after some pregnant individuals showed signs of folliculitis that were different than seen before. The inflammation was thought to be caused by hormonal imbalance, infection from bacteria, fungi, viruses or even an ingrown hair. However, there is no known definitive cause as of yet. These bumps usually begin on the belly and then spread to upper regions of the body as well as the thighs.
Keratosis pilaris atropicans is a group of idiopathic genodermatoses that consists of three unique clinical entities: atrophoderma vermiculatum, keratosis follicularis spinulosa decalvans, and keratosis pilaris atrophicans faciei.
Erythromelanosis follicularis faciei et colli is an erythematous pigmentary disease involving the follicles, characterized by a reddish-brown, sharply demarcated, symmetrical discoloration involving the preauricular and maxillary regions.
Traumatic anserine folliculosis is a curious gooseflesh-like follicular hyperkeratosis that may result from persistent pressure and lateral friction of one skin surface against another. Traumatic anserine folliculosis is caused by trauma. Topical keratolytics are the treatment of choice.

Majocchi's granuloma is a skin condition characterized by deep, pustular plaques, and is a form of tinea corporis. It is a localized form of fungal folliculitis. Lesions often have a pink and scaly central component with pustules or folliculocentric papules at the periphery. The name comes from Domenico Majocchi, who discovered the disorder in 1883. Majocchi was a professor of dermatology at the University of Parma and later the University of Bologna. The most common dermatophyte is called Trichophyton rubrum.
Childhood granulomatous periorificial dermatitis (CGPD), is a rare benign granulomatous skin disease of unknown cause. The disorder was first described in 1970 by Gianotti in a case series of five children. CGPD is more common in boys than girls.