Lichen planus (LP) is a chronic inflammatory and autoimmune disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, but is named for its appearance. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. The hue may be gray-brown in people with darker skin. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Actinic keratosis (AK), sometimes called solar keratosis or senile keratosis, is a pre-cancerous area of thick, scaly, or crusty skin. Actinic keratosis is a disorder of epidermal keratinocytes that is induced by ultraviolet (UV) light exposure. These growths are more common in fair-skinned people and those who are frequently in the sun. They are believed to form when skin gets damaged by UV radiation from the sun or indoor tanning beds, usually over the course of decades. Given their pre-cancerous nature, if left untreated, they may turn into a type of skin cancer called squamous cell carcinoma. Untreated lesions have up to a 20% risk of progression to squamous cell carcinoma, so treatment by a dermatologist is recommended.

Cutaneous T-cell lymphoma (CTCL) is a class of non-Hodgkin lymphoma, which is a type of cancer of the immune system. Unlike most non-Hodgkin lymphomas, CTCL is caused by a mutation of T cells. The cancerous T cells in the body initially migrate to the skin, causing various lesions to appear. These lesions change shape as the disease progresses, typically beginning as what appears to be a rash which can be very itchy and eventually forming plaques and tumors before spreading to other parts of the body.

Chlormethine, also known as mechlorethamine, mustine, HN2, and embikhin (эмбихин), is a nitrogen mustard sold under the brand name Mustargen among others. It is the prototype of alkylating agents, a group of anticancer chemotherapeutic drugs. It works by binding to DNA, crosslinking two strands and preventing cell duplication. It binds to the N7 nitrogen on the DNA base guanine. As the chemical is a blister agent, its use is strongly restricted within the Chemical Weapons Convention where it is classified as a Schedule 1 substance.

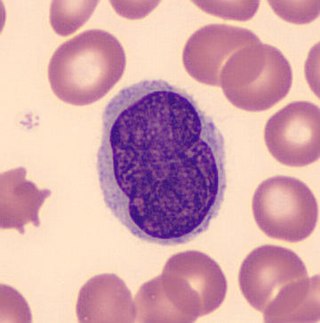
Sézary disease, or Sézary syndrome, is a type of cutaneous T-cell lymphoma that was first described by Albert Sézary. The affected T cells, known as Sézary's cells or Lutzner cells, have pathological quantities of mucopolysaccharides. Sézary disease is sometimes considered a late stage of mycosis fungoides with lymphadenopathy.

Sweet syndrome (SS), or acute febrile neutrophilic dermatosis, is a skin disease characterized by the sudden onset of fever, an elevated white blood cell count, and tender, red, well-demarcated papules and plaques that show dense infiltrates by neutrophil granulocytes on histologic examination.

T-cell lymphoma is a rare form of cancerous lymphoma affecting T-cells. Lymphoma arises mainly from the uncontrolled proliferation of T-cells and can become cancerous.
Florid cutaneous papillomatosis (FCP), is an obligate paraneoplastic syndrome.
Large plaque parapsoriasis are skin lesions that may be included in the modern scheme of cutaneous conditions described as parapsoriasis. These lesions, called plaques, may be irregularly round-shaped to oval and are 10 cm (4 in) or larger in diameter. They can be very thin plaques that are asymptomatic or mildly pruritic. Large-plaque parapsoriasis is a common associate of retiform parapsoriasis, can be accompanied by poikiloderma vasculare atrophicans, and can in rare occasions be a precursor to cutaneous T-cell lymphoma.
Pagetoid reticulosis is a cutaneous condition, an uncommon lymphoproliferative disorder, sometimes considered a form of mycosis fungoides.
Granulomatous slack skin (GSS) is a rare cutaneous condition, a variant of lymphoma that typically presents in middle-aged adults.
Secondary cutaneous CD30+ large-cell lymphoma is a cutaneous condition that may arise in cases of mycosis fungoides, and in patients with lymphomatoid papulosis.
Pleomorphic T-cell lymphoma is a cutaneous condition characterized by a 5-year survival rate of 62%.
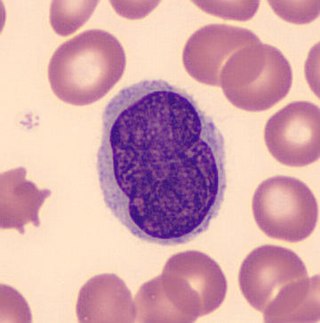
Lutzner cells were discovered by Marvin A. Lutzner, Lucien-Marie Pautrier, and Albert Sézary. These cells are described as the smaller forms of Sézary cells, or Sézary-Lutzner cells, and the two variants are recognised as being morphologically different. Aggregates of these cells in mycosis fungoides are known as a Pautrier's microabscesses. They are a form of T-lymphocytes that has been mutated This atypical form of T-lymphocytes contains T-cell receptors on the surface and is found in both the dermis and epidermis layers of the skin. Since Lutzner cells are a mutated form of T-lymphocytes, they develop in bone marrow and are transported to the thymus is order to mature. The production and maturation stages occur before the cell has developed a mutation. Lutzner cells can form cutaneous T-cell lymphoma, which is a form of skin cancer.

Poikiloderma vasculare atrophicans (PVA), is a cutaneous condition characterized by hypo- or hyperpigmentation, telangiectasia and skin atrophy. Other names for the condition include prereticulotic poikiloderma and atrophic parapsoriasis. The condition was first described by pioneer American pediatrician Abraham Jacobi in 1906. PVA causes areas of affected skin to appear speckled red and inflamed, yellowish and/or brown, gray or grayish-black, with scaling and a thinness that may be described as "cigarette paper". On the surface of the skin, these areas may range in size from small patches, to plaques, to neoplasms.
Senile pruritus is one of the most common conditions in the elderly or people over 65 years of age with an emerging itch that may be accompanied with changes in temperature and textural characteristics. In the elderly, xerosis, is the most common cause for an itch due to the degradation of the skin barrier over time. However, the cause of senile pruritus is not clearly known. Diagnosis is based on an elimination criteria during a full body examination that can be done by either a dermatologist or non-dermatologist physician.
Mogamulizumab, sold under the brand name Poteligeo, is a humanized, afucosylated monoclonal antibody targeting CC chemokine receptor 4 (CCR4). The U.S. Food and Drug Administration (FDA) approved it in August 2018 for treatment of relapsed or refractory mycosis fungoides and Sézary disease. It was approved in Japan in 2012, for the treatment of relapsed or refractory CCR4+ adult T-cell leukemia/lymphoma (ATCLL) and in 2014, for relapsed or refractory CCR4+ cutaneous T cell lymphoma (CTCL). The latter approval was based on study with 28 subjects.
Thomas S. Kupper is an American physician, academic, and clinician. His work with clinical and research experience spans dermatology, cutaneous oncology, and immunology. He is the Thomas B. Fitzpatrick Professor at Harvard Medical School, and chairs the Departments of Dermatology at Brigham and Women's Hospital. He also leads the Cutaneous Oncology Disease Center at the Dana Farber Cancer Institute.
Günter Burg is a German dermatologist. Born in Mayen, Germany, he holds German and Swiss citizenship. He has been married to Dr. Doris Burg-Nicklas, a neurologist, since 1968. They have two sons: Andreas and Thomas.