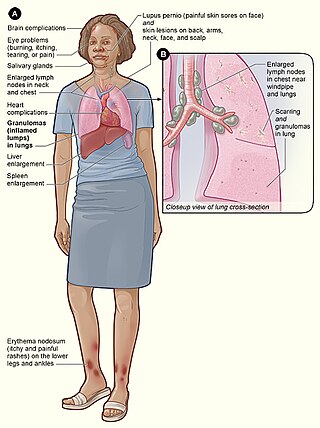
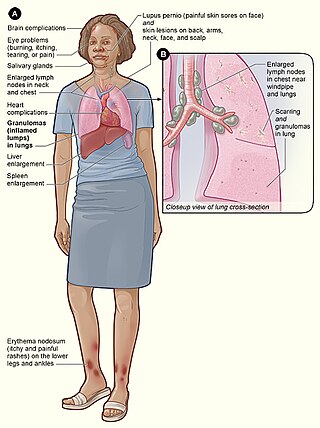
Sarcoidosis is a disease involving abnormal collections of inflammatory cells that form lumps known as granulomata. The disease usually begins in the lungs, skin, or lymph nodes. Less commonly affected are the eyes, liver, heart, and brain, though any organ can be affected. The signs and symptoms depend on the organ involved. Often, no, or only mild, symptoms are seen. When it affects the lungs, wheezing, coughing, shortness of breath, or chest pain may occur. Some may have Löfgren syndrome with fever, large lymph nodes, arthritis, and a rash known as erythema nodosum.

A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious organisms including bacteria and fungi, as well as other materials such as foreign objects, keratin, and suture fragments.

Panniculitis is a group of diseases whose hallmark is inflammation of subcutaneous adipose tissue. Symptoms include tender skin nodules, and systemic signs such as weight loss and fatigue.

Neurosarcoidosis refers to a type of sarcoidosis, a condition of unknown cause featuring granulomas in various tissues, in this type involving the central nervous system. Neurosarcoidosis can have many manifestations, but abnormalities of the cranial nerves are the most common. It may develop acutely, subacutely, and chronically. Approximately 5–10 percent of people with sarcoidosis of other organs develop central nervous system involvement. Only 1 percent of people with sarcoidosis will have neurosarcoidosis alone without involvement of any other organs. Diagnosis can be difficult, with no test apart from biopsy achieving a high accuracy rate. Treatment is with immunosuppression. The first case of sarcoidosis involving the nervous system was reported in 1905.

Clofazimine, sold under the brand name Lamprene, is a medication used together with rifampicin and dapsone to treat leprosy. It is specifically used for multibacillary (MB) leprosy and erythema nodosum leprosum. Evidence is insufficient to support its use in other conditions though a retrospective study found it 95% effective in the treatment of Mycobacterium avium complex (MAC) when administered with a macrolide and ethambutol, as well as the drugs amikacin and clarithromycin. However, in the United States, clofazimine is considered an orphan drug, is unavailable in pharmacies, and its use in the treatment of MAC is overseen by the Food and Drug Administration. It is taken orally.

Lupus vulgaris are painful cutaneous tuberculosis skin lesions with nodular appearance, most often on the face around the nose, eyelids, lips, cheeks, ears and neck. It is the most common Mycobacterium tuberculosis skin infection. The lesions may ultimately develop into disfiguring skin ulcers if left untreated.
Löfgren syndrome is a type of acute sarcoidosis, an inflammatory disorder characterized by swollen lymph nodes in the chest, tender red nodules on the shins, fever and arthritis. It is more common in women than men, and is more frequent in those of Scandinavian, Irish, African and Puerto Rican heritage. It was described in 1953 by Sven Halvar Löfgren, a Swedish clinician. Some have considered the condition to be imprecisely defined.

Prurigo nodularis (PN), also known as nodular prurigo, is a skin disorder characterized by pruritic (itchy), nodular lesions, which commonly appear on the trunk, arms and legs. Patients often present with multiple excoriated nodules caused by chronic scratching. Although the exact cause of PN is unknown, PN is associated with other dermatologic conditions such as untreated or severe atopic dermatitis and systemic causes of pruritus including liver disease and end stage kidney disease. The goal of treatment in PN is to decrease itching. PN is also known as Hyde prurigo nodularis, or Picker's nodules.

Erythema annulare centrifugum (EAC), is a descriptive term for a class of skin lesion presenting redness (erythema) in a ring form (anulare) that spreads from a center (centrifugum). It was first described by Darier in 1916. Many different terms have been used to classify these types of lesions and it is still controversial on what exactly defines EAC. Some of the types include annular erythema, erythema perstans, erythema gyratum perstans, erythema gyratum repens, darier erythema and erythema figuratum perstans.
Lupus erythematosus panniculitis presents with subcutaneous nodules that are commonly firm, sharply defined and nontender.
Recurrent palmoplantar hidradenitis, also known as idiopathic palmoplantar hidradenitis, idiopathic plantar hidradenitis, painful plantar erythema, palmoplantar eccrine hidradenitis, and plantar panniculitis, is primarily a disorder of healthy children and young adults, characterized by lesions that are primarily painful, subcutaneous nodules on the plantar surface, resembling erythema nodosum.

Erythema dyschromicum perstans is an uncommon skin condition with peak age of onset being young adults, but it may also be seen in children or adults of any age. EDP is characterized by hyperpigmented macules that are ash-grey in color and may vary in size and shape. While agents such as certain medications, radiographic contrast, pesticides, infection with parasites, and HIV have been implicated in the occurrence of this disease, the cause of this skin disease remains unknown.
Granuloma multiforme is a cutaneous condition most commonly seen in central Africa, and rarely elsewhere, characterized by skin lesions that are on the upper trunk and arms in sun-exposed areas. It may be confused with tuberculoid leprosy, with which it has clinical similarities. The condition was first noted by Gosset in the 1940s, but it was not until 1964 that Leiker coined the term to describe "a disease resembling leprosy" in his study in Nigeria.

Nakajo syndrome, also called nodular erythema with digital changes, is a rare autosomal recessive congenital disorder first reported in 1939 by A. Nakajo in the offspring of consanguineous parents. The syndrome can be characterized by erythema, loss of body fat in the upper part of the body, and disproportionately large eyes, ears, nose, lips, and fingers.
Jacob Sheskin, sometimes written as Sheskin Jacob was a Russian-born Israeli physician best known for his 1964 serendipitous discovery that thalidomide can be used as a treatment for leprosy at Hadassah University in Jerusalem.
Weber–Christian disease is a cutaneous condition characterized by recurrent subcutaneous nodules that heal with depression of the overlying skin.
Mosuke Murata was a Japanese dermatologist and was the designator of erythema nodosum leprosum (ENL)(1912), the type 2 lepra reaction.

Behçet's disease (BD) is a type of inflammatory disorder which affects multiple parts of the body. The most common symptoms include painful sores on the mucous membranes of the mouth and other parts of the body, inflammation of parts of the eye, and arthritis. The sores can last from a few days, up to a week or more. Less commonly there may be inflammation of the brain or spinal cord, blood clots, aneurysms, or blindness. Often, the symptoms come and go.

Sarcoidosis, an inflammatory disease, involves the skin in about 25% of patients. The most common lesions are erythema nodosum, plaques, maculopapular eruptions, subcutaneous nodules, and lupus pernio. Treatment is not required, since the lesions usually resolve spontaneously in two to four weeks. Although it may be disfiguring, cutaneous sarcoidosis rarely causes major problems.