Carcinoma is a malignancy that develops from epithelial cells. Specifically, a carcinoma is a cancer that begins in a tissue that lines the inner or outer surfaces of the body, and that arises from cells originating in the endodermal, mesodermal or ectodermal germ layer during embryogenesis.

The parotid gland is a major salivary gland in many animals. In humans, the two parotid glands are present on either side of the mouth and in front of both ears. They are the largest of the salivary glands. Each parotid is wrapped around the mandibular ramus, and secretes serous saliva through the parotid duct into the mouth, to facilitate mastication and swallowing and to begin the digestion of starches. There are also two other types of salivary glands; they are submandibular and sublingual glands. Sometimes accessory parotid glands are found close to the main parotid glands.
An oncocytoma is a tumor made up of oncocytes, epithelial cells characterized by an excessive amount of mitochondria, resulting in an abundant acidophilic, granular cytoplasm. The cells and the tumor that they compose are often benign but sometimes may be premalignant or malignant.
The International Classification of Diseases for Oncology (ICD-O) is a domain-specific extension of the International Statistical Classification of Diseases and Related Health Problems for tumor diseases. This classification is widely used by cancer registries.

Hemangioendotheliomas are a family of vascular neoplasms of intermediate malignancy.

A Hürthle cell is a cell in the thyroid that is often associated with Hashimoto's thyroiditis as well as benign and malignant tumors. This version is a relatively rare form of differentiated thyroid cancer, accounting for only 3-10% of all differentiated thyroid cancers. Oncocytes in the thyroid are often called Hürthle cells. Although the terms oncocyte, oxyphilic cell, and Hürthle cell are used interchangeably, Hürthle cell is used only to indicate cells of thyroid follicular origin.

Hürthle cell neoplasm is a rare tumor of the thyroid, typically seen in women between the ages of 70 and 80 years old. When benign, it is called a Hürthle cell adenoma, and when malignant it is called a Hürthle cell carcinoma. Hürthle cell adenoma is characterized by a mass of benign Hürthle cells. Typically such a mass is removed because it is not easy to predict whether it will transform into the malignant counterpart of Hürthle cell carcinoma, which is a subtype of follicular thyroid cancer.

Hidradenoma refers to a benign adnexal tumor of the apical sweat gland. These are 1–3 cm translucent blue cystic nodules. It usually presents as a single, small skin-colored lesion, and may be considered closely related to or a variant of poromas. Hidradenomas are often sub-classified based on subtle histologic differences, for example:

Myoepithelial cells are cells usually found in glandular epithelium as a thin layer above the basement membrane but generally beneath the luminal cells. These may be positive for alpha smooth muscle actin and can contract and expel the secretions of exocrine glands. They are found in the sweat glands, mammary glands, lacrimal glands, and salivary glands. Myoepithelial cells in these cases constitute the basal cell layer of an epithelium that harbors the epithelial progenitor. In the case of wound healing, myoepithelial cells reactively proliferate. Presence of myoepithelial cells in a hyperplastic tissue proves the benignity of the gland and, when absent, indicates cancer. Only rare cancers like adenoid cystic carcinomas contains myoepithelial cells as one of the malignant components.

A papillary hidradenoma, also termed hidradenoma papilliferum or mammary-like gland adenoma of the vulva, is a rare, but nonetheless most common benign tumor that occurs in and between anal and genital regions of females. These hidradenomas are sharply circumscribed, nodular tumors that usually develop in women's anogenital area but uncommonly occur in other sites in women and men. Papillary hidradenomas that develop outside of the anogenital region are termed ecctopic papillary hidradenomas or ectopic hidradenoma papilliferums.

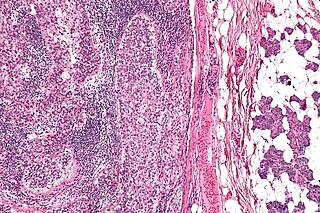
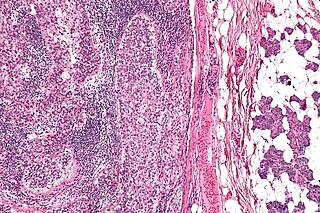
Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Sebaceous carcinoma, also known as sebaceous gland carcinoma (SGc), sebaceous cell carcinoma, and meibomian gland carcinoma is an uncommon malignant cutaneous tumor. Most are typically about 1.4 cm at presentation. SGc originates from sebaceous glands in the skin and, therefore, may originate anywhere in the body where these glands are found. SGc can be divided into 2 types: periocular and extraocular. The periocular region is rich in sebaceous glands making it a common site of origin. The cause of these lesions in the vast majority of cases is unknown. Occasional cases may be associated with Muir-Torre syndrome. SGc accounts for approximately 0.7% of all skin cancers, and the incidence of SGc is highest in Caucasian, Asian, and Indian populations. Due to the rarity of this tumor and variability in clinical and histological presentation, SGc is often misdiagnosed as an inflammatory condition or a more common neoplasm. SGc is commonly treated with wide local excision or Mohs micrographic surgery, and the relative survival rates at 5 and 10 years are 92.72 and 86.98%, respectively.

In medicine, desmoplasia is the growth of fibrous connective tissue. It is also called a desmoplastic reaction to emphasize that it is secondary to an insult. Desmoplasia may occur around a neoplasm, causing dense fibrosis around the tumor, or scar tissue (adhesions) within the abdomen after abdominal surgery.

Poromas are rare, benign, cutaneous adnexal tumors. Cutaneous adnexal tumors are a group of skin tumors consisting of tissues that have differentiated towards one or more of the four primary adnexal structures found in normal skin: hair follicles, sebaceous sweat glands, apocrine sweat glands, and eccrine sweat glands. Poromas are eccrine or apocrine sweat gland tumors derived from the cells in the terminal portion of these glands' ducts. This part of the sweat gland duct is termed the acrosyringium and had led to grouping poromas in the acrospiroma class of skin tumors. Here, poromas are regarded as distinct sweat gland tumors that differ from other sweat gland tumors by their characteristic clinical presentations, microscopic histopathology, and the genetic mutations that their neoplastic cells have recently been found to carry.
Porocarcinoma (PCA) is a rare form of skin cancer that develops in eccrine sweat glands, i.e. the body's widely distributed major type of sweat glands, as opposed to the apocrine sweat glands which are located primarily in the armpits and perineal area. This cancer typically develops in individuals as a single cutaneous tumor in the intraepidermal spiral part of these sweat glands' ducts at or near to where they open on the skin's surface. PCA tumors are classified as one form of the cutaneous adnexal tumors; in a study of 2,205 cases, PCA was the most common (11.8%) form of these tumors.

Spiradenomas (SA) are rare, benign cutaneous adnexal tumors that may progress to become their malignant counterparts, i.e. spiradenocarcinomas (SAC). Cutaneous adnexal tumors are a group of skin tumors consisting of tissues that have differentiated towards one of the four primary adnexal structures found in normal skin: hair follicles, sebaceous sweat glands, apocrine sweat glands, and eccrine sweat glands. SA and SAC tumors were regarded as eccrine gland tumors and termed eccrine spiradenomas and eccrine spiradenocarcinomas, respectively. However, more recent studies have found them to be hair follicle tumors and commonly term them spiradenomas and spiradenocarcinomas, respectively. Further confusing the situation, SA-like and SAC-like tumors are also 1) manifestations of the inherited disorder, CYLD cutaneous syndrome (CCS), and 2) have repeatedly been confused with an entirely different tumor, adenoid cystic carcinomas of the salivary gland. Here, SA and SAC are strictly defined as sporadic hair follicle tumors that do not include the hereditary CCS spiradenomas and heridtary spiradenocarcinoms of CCS or the adenoid cystic carcinomas.

Eccrine carcinoma is a rare skin condition characterized by a plaque or nodule on the scalp, trunk, or extremities. It originates from the eccrine sweat glands of the skin, accounting for less than 0.01% of diagnosed cutaneous malignancies. Eccrine carcinoma tumors are locally aggressive, with a high rate of recurrence. Lack of reliable immunohistochemical markers and similarity to other common tumors has made identification of eccrine carcinoma difficult.

Sclerosing polycystic adenosis is a rare salivary gland tumor first described in 1996 by Dr. Brion Smith. The major salivary glands, specifically the parotid gland and the submandibular gland, are affected most commonly. Patients usually come to clinical attention with a mass or swelling in their salivary glands in the 5th decade of life, with females affected much more commonly than males. Nearly all of the cases reported so far have a benign behavior, although there is a single case that has had an associated malignant transformation.
Vulvar tumors are those neoplasms of the vulva. Vulvar and vaginal neoplasms make up a small percentage (3%) of female genital cancers. They can be benign or malignant. Vulvar neoplasms are divided into cystic or solid lesions and other mixed types. Vulvar cancers are those malignant neoplasms that originate from vulvar epithelium, while vulvar sarcomas develop from non-epithelial cells such as bone, cartilage, fat, muscle, blood vessels, or other connective or supportive tissue. Epithelial and mesenchymal tissue are the origin of vulvar tumors.