Plague is an infectious disease caused by the bacterium Yersinia pestis. Symptoms include fever, weakness and headache. Usually this begins one to seven days after exposure. There are three forms of plague, each affecting a different part of the body and causing associated symptoms. Pneumonic plague infects the lungs, causing shortness of breath, coughing and chest pain; bubonic plague affects the lymph nodes, making them swell; and septicemic plague infects the blood and can cause tissues to turn black and die.
Brucellosis is a zoonosis caused by ingestion of unpasteurized milk from infected animals, or close contact with their secretions. It is also known as undulant fever, Malta fever, and Mediterranean fever.

Septicemic plague is one of the three forms of plague, and is caused by Yersinia pestis, a gram-negative species of bacterium. Septicemic plague is a systemic disease involving infection of the blood and is most commonly spread by bites from infected fleas. Septicemic plague can cause disseminated intravascular coagulation and is always fatal when untreated. The other varieties of the plague are bubonic plague and pneumonic plague.

A broad-spectrum antibiotic is an antibiotic that acts on the two major bacterial groups, Gram-positive and Gram-negative, or any antibiotic that acts against a wide range of disease-causing bacteria. These medications are used when a bacterial infection is suspected but the group of bacteria is unknown or when infection with multiple groups of bacteria is suspected. This is in contrast to a narrow-spectrum antibiotic, which is effective against only a specific group of bacteria. Although powerful, broad-spectrum antibiotics pose specific risks, particularly the disruption of native, normal bacteria and the development of antimicrobial resistance. An example of a commonly used broad-spectrum antibiotic is ampicillin.
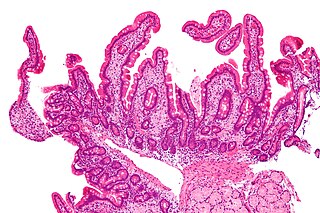
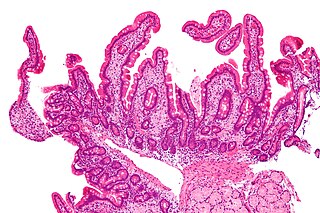
Whipple's disease is a rare systemic infectious disease caused by the bacterium "Tropheryma whipplei". First described by George Hoyt Whipple in 1907 and commonly considered as a gastrointestinal disorder, Whipple's disease primarily causes malabsorption, but may affect any part of the human body, including the heart, brain, joints, skin, lungs and the eyes. Weight loss, diarrhea, joint pain, and arthritis are common presenting symptoms, but the presentation can be highly variable in certain individuals, and about 15% of patients do not have the standard signs and symptoms.

Streptobacillus is a genus of fastidious microaerophilic Gram-negative bacteria, which grow in culture as rods in chains.

Erysipelothrix rhusiopathiae is a Gram-positive, catalase-negative, rod-shaped, non-spore-forming, nonacid-fast, nonmotile bacterium. Distributed worldwide, E. rhusiopathiae is primarily considered an animal pathogen, causing the disease known as erysipelas that may affect a wide range of animals. Pigs, turkeys and laying hens are most commonly affected, but cases have been reported in other mammals, birds, fish, and reptiles. In pigs, the disease is known as diamond skin disease. The bacterium can also cause zoonotic infections in humans, called erysipeloid. The human disease called erysipelas is not caused by E. rhusiopathiae, but by various members of the genus Streptococcus.

Bacterial pneumonia is a type of pneumonia caused by bacterial infection.
Tick-borne diseases, which afflict humans and other animals, are caused by infectious agents transmitted by tick bites. They are caused by infection with a variety of pathogens, including rickettsia and other types of bacteria, viruses, and protozoa. The economic impact of tick-borne diseases is considered to be substantial in humans, and tick-borne diseases are estimated to affect ~80 % of cattle worldwide. Most of these pathogens require passage through vertebrate hosts as part of their life cycle. Tick-borne infections in humans, farm animals, and companion animals are primarily associated with wildlife animal reservoirs. many tick-borne infections in humans involve a complex cycle between wildlife animal reservoirs and tick vectors. The survival and transmission of these tick-borne viruses are closely linked to their interactions with tick vectors and host cells. These viruses are classified into different families, including Asfarviridae, Reoviridae, Rhabdoviridae, Orthomyxoviridae, Bunyaviridae, and Flaviviridae.
Rat-bite fever (RBF) is an acute, febrile human illness caused by bacteria transmitted by rodents, in most cases, which is passed from rodent to human by the rodent's urine or mucous secretions. Alternative names for rat-bite fever include streptobacillary fever, streptobacillosis, spirillary fever, bogger, and epidemic arthritic erythema. It is a rare disease spread by infected rodents and caused by two specific types of bacteria:
- Streptobacillus moniliformis, the only reported bacteria that causes RBF in North America
- Spirillum minus, common in Asia. Most cases occur in Japan, but specific strains of the disease are present in the United States, Europe, Australia, and Africa.

Brucella is a genus of Gram-negative bacteria, named after David Bruce (1855–1931). They are small, nonencapsulated, nonmotile, facultatively intracellular coccobacilli.
Sodoku is a bacterial zoonotic disease. It is caused by the Gram-negative rod Spirillum minus. It is a form of rat-bite fever (RBF).

Eikenella corrodens is a Gram-negative facultative anaerobic bacillus that can cause severe invasive disease in humans. It was first identified by M. Eiken in 1958, who called it Bacteroides corrodens. E. corrodens is a rare pericarditis associated pathogen. It is a fastidious, slow growing, human commensal bacillus, capable of acting as an opportunistic pathogen and causing abscesses in several anatomical sites, including the liver, lung, spleen, and submandibular region. E. corrodens could independently cause serious infection in both immunocompetent and immunocompromised hosts.
Capnocytophaga canimorsus is a fastidious, slow-growing, Gram-negative rod of the genus Capnocytophaga. It is a commensal bacterium in the normal gingival flora of canine and feline species, but can cause illness in humans. Transmission may occur through bites, licks, or even close proximity with animals. C. canimorsus generally has low virulence in healthy individuals, but has been observed to cause severe, even grave, illness in persons with pre-existing conditions. The pathogenesis of C. canimorsus is still largely unknown, but increased clinical diagnoses have fostered an interest in the bacillus. Treatment with antibiotics is effective in most cases, but the most important yet basic diagnostic tool available to clinicians remains the knowledge of recent exposure to canines or felines.

Medical microbiology, the large subset of microbiology that is applied to medicine, is a branch of medical science concerned with the prevention, diagnosis and treatment of infectious diseases. In addition, this field of science studies various clinical applications of microbes for the improvement of health. There are four kinds of microorganisms that cause infectious disease: bacteria, fungi, parasites and viruses, and one type of infectious protein called prion.
Ehrlichiosis ewingii infection is an infectious disease caused by an intracellular bacteria, Ehrlichia ewingii. The infection is transmitted to humans by the tick, Amblyomma americanum. This tick can also transmit Ehrlichia chaffeensis, the bacteria that causes human monocytic ehrlichiosis (HME).
Rickettsia typhi is a small, aerobic, obligate intracellular, rod shaped gram negative bacterium. It belongs to the typhus group of the Rickettsia genus, along with R. prowazekii. R. typhi has an uncertain history, as it may have long gone shadowed by epidemic typhus. This bacterium is recognized as a biocontainment level 2/3 organism. R. typhi is a flea-borne disease that is best known to be the causative agent for the disease murine typhus, which is an endemic typhus in humans that is distributed worldwide. As with all rickettsial organisms, R. typhi is a zoonotic agent that causes the disease murine typhus, displaying non-specific mild symptoms of fevers, headaches, pains and rashes. There are two cycles of R. typhi transmission from animal reservoirs containing R. typhi to humans: a classic rat-flea-rat cycle that is most well studied and common, and a secondary periodomestic cycle that could involve cats, dogs, opossums, sheep, and their fleas.

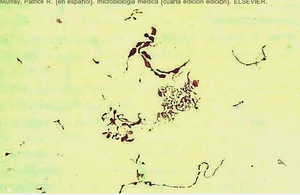
Streptobacillus moniliformis is a non-motile, Gram-negative rod-shaped bacterium that is a member of the family Leptotrichiaceae. The genome of S. moniliformis is one of two completed sequences of the order Fusobacteriales. Its name comes from the Greek word streptos for "curved" or "twisted", and the Latin word bacillus meaning "small rod" and moniliformis for "necklace". S. moniliformis is microaerophilic, requiring less oxygen than is present in the atmosphere for its growth.
Pasteurella canis is a Gram-negative, nonmotile, penicillin-sensitive coccobacillus of the family Pasteurellaceae. Bacteria from this family cause zoonotic infections in humans, which manifest themselves as skin or soft-tissue infections after an animal bite. It has been known to cause serious disease in immunocompromised patients.
There are many circumstances during dental treatment where antibiotics are prescribed by dentists to prevent further infection. The most common antibiotic prescribed by dental practitioners is penicillin in the form of amoxicillin, however many patients are hypersensitive to this particular antibiotic. Therefore, in the cases of allergies, erythromycin is used instead.