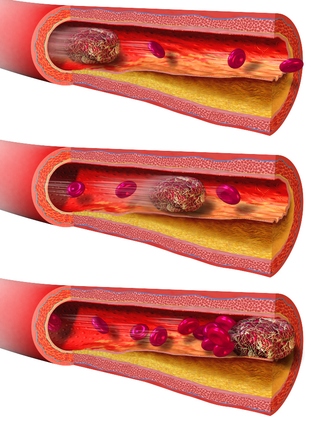
An embolism is the lodging of an embolus, a blockage-causing piece of material, inside a blood vessel. The embolus may be a blood clot (thrombus), a fat globule, a bubble of air or other gas, amniotic fluid, or foreign material.
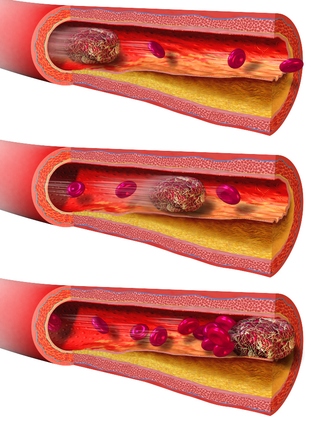
An embolus is an unattached mass that travels through the bloodstream and is capable of creating blockages. When an embolus occludes a blood vessel, it is called an embolism or embolic event. There are a number of different types of emboli, including blood clots, cholesterol plaque or crystals, fat globules, gas bubbles, and foreign bodies, which can result in different types of embolisms.

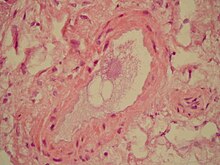
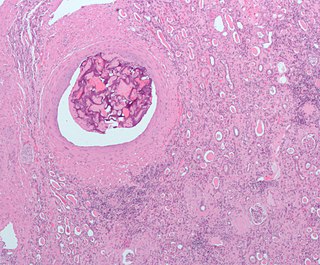
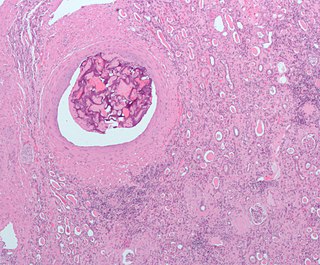
A thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to stop and prevent further bleeding, but can be harmful in thrombosis, when a clot obstructs blood flow through healthy blood vessels in the circulatory system.

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered state of consciousness due to ischemia in the brain.
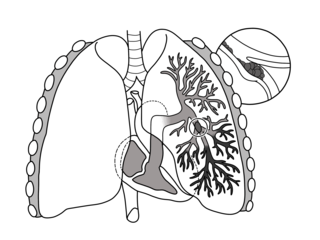
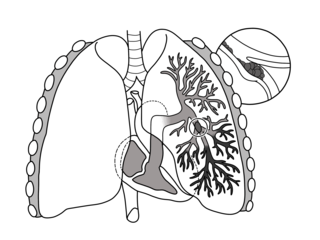
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.

Cyanosis is the change of body tissue color to a bluish-purple hue, as a result of decrease in the amount of oxygen bound to the hemoglobin in the red blood cells of the capillary bed. Cyanosis is apparent usually in the body tissues covered with thin skin, including the mucous membranes, lips, nail beds, and ear lobes. Some medications may cause discoloration such as medications containing amiodarone or silver. Furthermore, mongolian spots, large birthmarks, and the consumption of food products with blue or purple dyes can also result in the bluish skin tissue discoloration and may be mistaken for cyanosis. Appropriate physical examination and history taking is a crucial part to diagnose cyanosis. Management of cyanosis involves treating the main cause, as cyanosis isn’t a disease, it is a symptom.

An air embolism, also known as a gas embolism, is a blood vessel blockage caused by one or more bubbles of air or other gas in the circulatory system. Air can be introduced into the circulation during surgical procedures, lung over-expansion injury, decompression, and a few other causes. In flora, air embolisms may also occur in the xylem of vascular plants, especially when suffering from water stress.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this does not naturally close after birth it is referred to as a patent (open) foramen ovale (PFO). It is common in patients with a congenital atrial septal aneurysm (ASA).

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
An embolus, is described as a free-floating mass, located inside blood vessels that can travel from one site in the blood stream to another. An embolus can be made up of solid, liquid, or gas. Once these masses get "stuck" in a different blood vessel, it is then known as an "embolism." An embolism can cause ischemia—damage to an organ from lack of oxygen. A paradoxical embolism is a specific type of embolism in which the embolus travels from the right side of the heart to the left side of the heart and lodges itself in a blood vessel known as an artery. Thus, it is termed "paradoxical" because the embolus lands in an artery, rather than a vein.

A CT pulmonary angiogram (CTPA) is a medical diagnostic test that employs computed tomography (CT) angiography to obtain an image of the pulmonary arteries. Its main use is to diagnose pulmonary embolism (PE). It is a preferred choice of imaging in the diagnosis of PE due to its minimally invasive nature for the patient, whose only requirement for the scan is an intravenous line.
Pediatric advanced life support (PALS) is a course offered by the American Heart Association (AHA) for health care providers who take care of children and infants in the emergency room, critical care and intensive care units in the hospital, and out of hospital. The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.

Cholesterol embolism occurs when cholesterol is released, usually from an atherosclerotic plaque, and travels as an embolus in the bloodstream to lodge causing an obstruction in blood vessels further away. Most commonly this causes skin symptoms, gangrene of the extremities and sometimes kidney failure; problems with other organs may arise, depending on the site at which the cholesterol crystals enter the bloodstream. When the kidneys are involved, the disease is referred to as atheroembolic renal disease. The diagnosis usually involves biopsy from an affected organ. Cholesterol embolism is treated by removing the cause and giving supportive therapy; statin drugs have been found to improve the prognosis.

In transfusion medicine, transfusion-associated circulatory overload is a transfusion reaction resulting in signs or symptoms of excess fluid in the circulatory system (hypervolemia) within 12 hours after transfusion. The symptoms of TACO can include shortness of breath (dyspnea), low blood oxygen levels (hypoxemia), leg swelling, high blood pressure (hypertension), and a high heart rate (tachycardia).
Embolectomy is the emergency interventional or surgical removal of emboli which are blocking blood circulation. It usually involves removal of thrombi, and is then referred to as thromboembolectomy or thrombectomy. Embolectomy is an emergency procedure often as the last resort because permanent occlusion of a significant blood flow to an organ leads to necrosis. Other involved therapeutic options are anticoagulation and thrombolysis.

Purtscher's retinopathy is a disease where part of the eye (retina) is damaged. Usually associated with severe head injuries, it may also occur with other types of trauma, such as long bone fractures, or with several non-traumatic systemic diseases. However, the exact cause of the disease is not well understood. There are no treatments specific for Purtscher's retinopathy, and the prognosis varies. The disease can threaten vision, sometimes causing temporary or permanent blindness.

Arterial embolism is a sudden interruption of blood flow to an organ or body part due to an embolus adhering to the wall of an artery blocking the flow of blood, the major type of embolus being a blood clot (thromboembolism). Sometimes, pulmonary embolism is classified as arterial embolism as well, in the sense that the clot follows the pulmonary artery carrying deoxygenated blood away from the heart. However, pulmonary embolism is generally classified as a form of venous embolism, because the embolus forms in veins. Arterial embolism is the major cause of infarction.