In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.
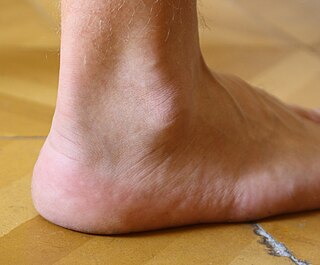
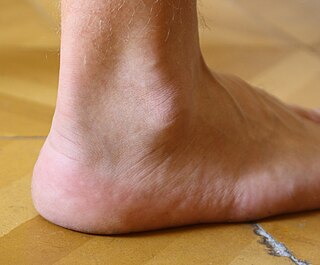
The ankle, the talocrural region or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joint. The movements produced at this joint are dorsiflexion and plantarflexion of the foot. In common usage, the term ankle refers exclusively to the ankle region. In medical terminology, "ankle" can refer broadly to the region or specifically to the talocrural joint.

A bone fracture is a medical condition in which there is a partial or complete break in the continuity of any bone in the body. In more severe cases, the bone may be broken into several fragments, known as a comminuted fracture. A bone fracture may be the result of high force impact or stress, or a minimal trauma injury as a result of certain medical conditions that weaken the bones, such as osteoporosis, osteopenia, bone cancer, or osteogenesis imperfecta, where the fracture is then properly termed a pathologic fracture.

A Lisfranc injury, also known as Lisfranc fracture, is an injury of the foot in which one or more of the metatarsal bones are displaced from the tarsus.

The shoulder joint is structurally classified as a synovial ball-and-socket joint and functionally as a diarthrosis and multiaxial joint. It involves an articulation between the glenoid fossa of the scapula and the head of the humerus. Due to the very loose joint capsule that gives a limited interface of the humerus and scapula, it is the most mobile joint of the human body.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.

A hip dislocation is when the thighbone (femur) separates from the hip bone (pelvis). Specifically it is when the ball–shaped head of the femur separates from its cup–shaped socket in the hip bone, known as the acetabulum. The joint of the femur and pelvis is very stable, secured by both bony and soft-tissue constraints. With that, dislocation would require significant force which typically results from significant trauma such as from a motor vehicle collision or from a fall from elevation. Hip dislocations can also occur following a hip replacement or from a developmental abnormality known as hip dysplasia.

Hypermobility, also known as double-jointedness, describes joints that stretch farther than normal. For example, some hypermobile people can bend their thumbs backwards to their wrists and bend their knee joints backwards, put their leg behind the head or perform other contortionist "tricks". It can affect one or more joints throughout the body.

A separated shoulder, also known as acromioclavicular joint injury, is a common injury to the acromioclavicular joint. The AC joint is located at the outer end of the clavicle where it attaches to the acromion of the scapula. Symptoms include non-radiating pain which may make it difficult to move the shoulder. The presence of swelling or bruising and a deformity in the shoulder is also common depending on how severe the dislocation is.

A dislocated shoulder is a condition in which the head of the humerus is detached from the glenoid fossa. Symptoms include shoulder pain and instability. Complications may include a Bankart lesion, Hill-Sachs lesion, rotator cuff tear, or injury to the axillary nerve.

A calcaneal fracture is a break of the calcaneus. Symptoms may include pain, bruising, trouble walking, and deformity of the heel. It may be associated with breaks of the hip or back.
Shoulder surgery is a means of treating injured shoulders. Many surgeries have been developed to repair the muscles, connective tissue, or damaged joints that can arise from traumatic or overuse injuries to the shoulder.

A Bankart lesion is a type of shoulder injury that occurs following a dislocated shoulder. It is an injury of the anterior (inferior) glenoid labrum of the shoulder. When this happens, a pocket at the front of the glenoid forms that allows the humeral head to dislocate into it. It is an indication for surgery and often accompanied by a Hill-Sachs lesion, damage to the posterior humeral head.

A Hill–Sachs lesion, or Hill–Sachs fracture, is a cortical depression in the posterolateral head of the humerus. It results from forceful impaction of the humeral head against the anteroinferior glenoid rim when the shoulder is dislocated anteriorly.

Jammed finger is a colloquialism referring to a variety of injuries to the joints of the fingers, resulting from axial loading beyond that which the ligaments can withstand. Common parts of the finger susceptible to this type of injury are ligaments, joints, and bones. The severity of the damage to the finger increases with the magnitude of the force exerted by the external object on the fingertip. Toes may become jammed as well, with similar results.

A patellar dislocation is a knee injury in which the patella (kneecap) slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place. Complications may include a patella fracture or arthritis.

Orthopedic surgery is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal injuries, sports injuries, degenerative diseases, infections, bone tumours, and congenital limb deformities. Trauma surgery and traumatology is a sub-specialty dealing with the operative management of fractures, major trauma and the multiply-injured patient.
The treatment of broken bones and dislocated joints can be traced as far back as the Ancient Greeks. Hippocrates is credited with a method of reduction of a dislocated shoulder. 16th century Spanish texts talk about the Aztecs use of reduction of fractures using fir branches. The modern discipline of orthopaedics in trauma care developed during the course of World War I, but it was not until after World War II that orthopaedics became the dominant field treating fractures in much of the world. Today, the discipline encompasses conditions such as bone fractures and bone loss, as well as spinal pathology and joint disease.

A knee dislocation is an injury in which there is disruption of the knee joint between the tibia and the femur. Symptoms include pain and instability of the knee. Complications may include injury to an artery, most commonly the popliteal artery behind the knee, or compartment syndrome.