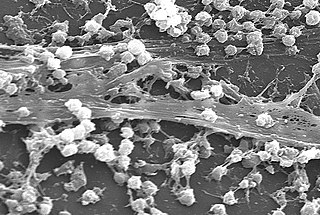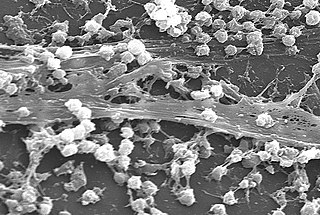
A biofilm is a syntrophic community of microorganisms in which cells stick to each other and often also to a surface. These adherent cells become embedded within a slimy extracellular matrix that is composed of extracellular polymeric substances (EPSs). The cells within the biofilm produce the EPS components, which are typically a polymeric combination of extracellular polysaccharides, proteins, lipids and DNA. Because they have a three-dimensional structure and represent a community lifestyle for microorganisms, they have been metaphorically described as "cities for microbes".

Waterhouse–Friderichsen syndrome (WFS) is defined as adrenal gland failure due to bleeding into the adrenal glands, commonly caused by severe bacterial infection. Typically, it is caused by Neisseria meningitidis.

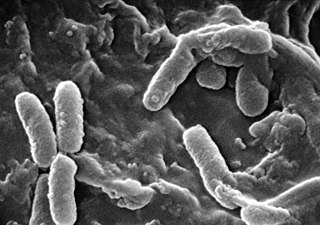
Pseudomonas is a genus of Gram-negative bacteria belonging to the family Pseudomonadaceae in the class Gammaproteobacteria. The 313 members of the genus demonstrate a great deal of metabolic diversity and consequently are able to colonize a wide range of niches. Their ease of culture in vitro and availability of an increasing number of Pseudomonas strain genome sequences has made the genus an excellent focus for scientific research; the best studied species include P. aeruginosa in its role as an opportunistic human pathogen, the plant pathogen P. syringae, the soil bacterium P. putida, and the plant growth-promoting P. fluorescens, P. lini, P. migulae, and P. graminis.

Folliculitis is the infection and inflammation of one or more hair follicles. The condition may occur anywhere on hair-covered skin. The rash may appear as pimples that come to white tips on the face, chest, back, arms, legs, buttocks, or head.

A nail disease or onychosis is a disease or deformity of the nail. Although the nail is a structure produced by the skin and is a skin appendage, nail diseases have a distinct classification as they have their own signs and symptoms which may relate to other medical conditions. Some nail conditions that show signs of infection or inflammation may require medical assistance.

Aztreonam, sold under the brand name Azactam among others, is an antibiotic used primarily to treat infections caused by gram-negative bacteria such as Pseudomonas aeruginosa. This may include bone infections, endometritis, intra abdominal infections, pneumonia, urinary tract infections, and sepsis. It is given by intravenous or intramuscular injection or by inhalation.

Colistin, also known as polymyxin E, is an antibiotic medication used as a last-resort treatment for multidrug-resistant Gram-negative infections including pneumonia. These may involve bacteria such as Pseudomonas aeruginosa, Klebsiella pneumoniae, or Acinetobacter. It comes in two forms: colistimethate sodium can be injected into a vein, injected into a muscle, or inhaled, and colistin sulfate is mainly applied to the skin or taken by mouth. Colistimethate sodium is a prodrug; it is produced by the reaction of colistin with formaldehyde and sodium bisulfite, which leads to the addition of a sulfomethyl group to the primary amines of colistin. Colistimethate sodium is less toxic than colistin when administered parenterally. In aqueous solutions it undergoes hydrolysis to form a complex mixture of partially sulfomethylated derivatives, as well as colistin. Resistance to colistin began to appear as of 2015.
Dermatophyte is a common label for a group of fungus of Arthrodermataceae that commonly causes skin disease in animals and humans. Traditionally, these anamorphic mold genera are: Microsporum, Epidermophyton and Trichophyton. There are about 40 species in these three genera. Species capable of reproducing sexually belong in the teleomorphic genus Arthroderma, of the Ascomycota. As of 2019 a total of nine genera are identified and new phylogenetic taxonomy has been proposed.
Multiple drug resistance (MDR), multidrug resistance or multiresistance is antimicrobial resistance shown by a species of microorganism to at least one antimicrobial drug in three or more antimicrobial categories. Antimicrobial categories are classifications of antimicrobial agents based on their mode of action and specific to target organisms. The MDR types most threatening to public health are MDR bacteria that resist multiple antibiotics; other types include MDR viruses, parasites.

Paronychia is an inflammation of the skin around the nail, which can occur suddenly, when it is usually due to the bacterium Staphylococcus aureus, or gradually when it is commonly caused by the fungus Candida albicans. The term is from Greek: παρωνυχία from para 'around', onyx 'nail', and the abstract noun suffix -ia.

Onychomycosis, also known as tinea unguium, is a fungal infection of the nail. Symptoms may include white or yellow nail discoloration, thickening of the nail, and separation of the nail from the nail bed. Fingernails may be affected, but it is more common for toenails. Complications may include cellulitis of the lower leg. A number of different types of fungus can cause onychomycosis, including dermatophytes and Fusarium. Risk factors include athlete's foot, other nail diseases, exposure to someone with the condition, peripheral vascular disease, and poor immune function. The diagnosis is generally suspected based on the appearance and confirmed by laboratory testing.

Pseudomonas aeruginosa is a common encapsulated, Gram-negative, aerobic–facultatively anaerobic, rod-shaped bacterium that can cause disease in plants and animals, including humans. A species of considerable medical importance, P. aeruginosa is a multidrug resistant pathogen recognized for its ubiquity, its intrinsically advanced antibiotic resistance mechanisms, and its association with serious illnesses – hospital-acquired infections such as ventilator-associated pneumonia and various sepsis syndromes. P. aeruginosa is able to selectively inhibit various antibiotics from penetrating its outer membrane - and has high resistance to several antibiotics, according to the World Health Organization P. aeruginosa poses one of the greatest threats to humans in terms of antibiotic resistance.
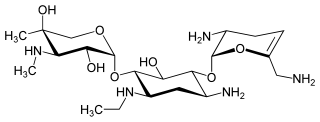
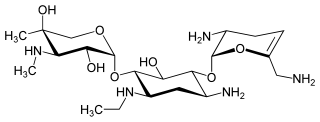
Netilmicin (1-N-ethylsisomicin) is a semisynthetic aminoglycoside antibiotic, and a derivative of sisomicin, produced by Micromonospora inyoensis. Aminoglycoside antibiotics have the ability to kill a wide variety of bacteria. Netilmicin is not absorbed from the gut and is therefore only given by injection or infusion. It is only used in the treatment of serious infections particularly those resistant to gentamicin.

Clobetasone (INN) is a corticosteroid used in dermatology, for treating such skin inflammation as seen in eczema, psoriasis and other forms of dermatitis, and ophthalmology. Topical clobetasone butyrate has shown minimal suppression of the hypothalamic–pituitary–adrenal axis.

Hot tub folliculitis, also called Pseudomonalfolliculitis or Pseudomonas aeruginosa folliculitis, is a common type of folliculitis featuring inflammation of hair follicles and surrounding skin.

Skin flora, also called skin microbiota, refers to microbiota that reside on the skin, typically human skin.
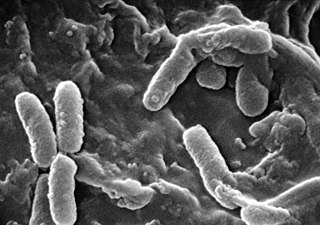
Pseudomonas infection refers to a disease caused by one of the species of the genus Pseudomonas.
Multidrug resistant Gram-negative bacteria are a type of Gram-negative bacteria with resistance to multiple antibiotics. They can cause bacteria infections that pose a serious and rapidly emerging threat for hospitalized patients and especially patients in intensive care units. Infections caused by MDR strains are correlated with increased morbidity, mortality, and prolonged hospitalization. Thus, not only do these bacteria pose a threat to global public health, but also create a significant burden to healthcare systems.

Otitis externa, also called swimmer's ear, is inflammation of the ear canal. It often presents with ear pain, swelling of the ear canal, and occasionally decreased hearing. Typically there is pain with movement of the outer ear. A high fever is typically not present except in severe cases.

Finafloxacin (Xtoro) is a fluoroquinolone antibiotic. In the United States, it is approved by the Food and Drug Administration to treat acute otitis externa caused by the bacteria Pseudomonas aeruginosa and Staphylococcus aureus.