Related Research Articles

Interstitial cystitis (IC), a type of bladder pain syndrome (BPS), is chronic pain in the bladder and pelvic floor of unknown cause. It is the urologic chronic pelvic pain syndrome of women. Symptoms include feeling the need to urinate right away, needing to urinate often, and pain with sex. IC/BPS is associated with depression and lower quality of life. Many of those affected also have irritable bowel syndrome and fibromyalgia.
A urinary tract infection (UTI) is an infection that affects part of the urinary tract. When it affects the lower urinary tract it is known as a bladder infection (cystitis) and when it affects the upper urinary tract it is known as a kidney infection (pyelonephritis). Symptoms from a lower urinary tract infection include pain with urination, frequent urination, and feeling the need to urinate despite having an empty bladder. Symptoms of a kidney infection include fever and flank pain usually in addition to the symptoms of a lower UTI. Rarely the urine may appear bloody. In the very old and the very young, symptoms may be vague or non-specific.

The bladder is a hollow organ in humans and other vertebrates that stores urine from the kidneys before disposal by urination. In humans the bladder is a distensible organ that sits on the pelvic floor. Urine enters the bladder via the ureters and exits via the urethra. The typical adult human bladder will hold between 300 and 500 ml before the urge to empty occurs, but can hold considerably more.

Prostatitis is an umbrella term for a variety of medical conditions that incorporate bacterial and non-bacterial origin illnesses in the pelvic region. In contrast with the plain meaning of the word, the diagnosis may not always include inflammation. Prostatitis is classified into acute, chronic, asymptomatic inflammatory prostatitis, and chronic pelvic pain syndrome.

Benign prostatic hyperplasia (BPH), also called prostate enlargement, is a noncancerous increase in size of the prostate gland. Symptoms may include frequent urination, trouble starting to urinate, weak stream, inability to urinate, or loss of bladder control. Complications can include urinary tract infections, bladder stones, and chronic kidney problems.
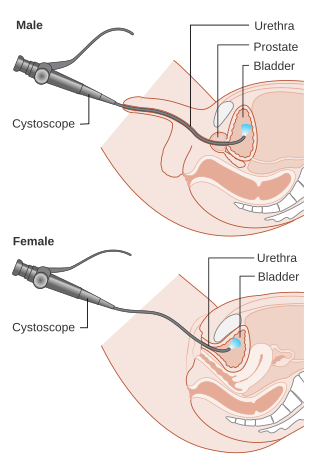
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

The ureters are tubes made of smooth muscle that propel urine from the kidneys to the urinary bladder. In a human adult, the ureters are usually 20–30 cm (8–12 in) long and around 3–4 mm (0.12–0.16 in) in diameter. The ureter is lined by urothelial cells, a type of transitional epithelium, and has an additional smooth muscle layer that assists with peristalsis in its lowest third.

A bladder stone is a stone found in the urinary bladder.

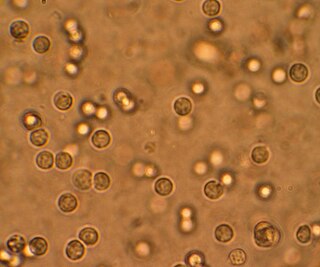
Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. "Gross hematuria" occurs when urine appears red, brown, or tea-colored due to the presence of blood. Hematuria may also be subtle and only detectable with a microscope or laboratory test. Blood that enters and mixes with the urine can come from any location within the urinary system, including the kidney, ureter, urinary bladder, urethra, and in men, the prostate. Common causes of hematuria include urinary tract infection (UTI), kidney stones, viral illness, trauma, bladder cancer, and exercise. These causes are grouped into glomerular and non-glomerular causes, depending on the involvement of the glomerulus of the kidney. But not all red urine is hematuria. Other substances such as certain medications and foods can cause urine to appear red. Menstruation in women may also cause the appearance of hematuria and may result in a positive urine dipstick test for hematuria. A urine dipstick test may also give an incorrect positive result for hematuria if there are other substances in the urine such as myoglobin, a protein excreted into urine during rhabdomyolysis. A positive urine dipstick test should be confirmed with microscopy, where hematuria is defined by three or more red blood cells per high power field. When hematuria is detected, a thorough history and physical examination with appropriate further evaluation can help determine the underlying cause.
Dysuria refers to painful or uncomfortable urination.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.

Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.

Hydronephrosis describes hydrostatic dilation of the renal pelvis and calyces as a result of obstruction to urine flow downstream. Alternatively, hydroureter describes the dilation of the ureter, and hydronephroureter describes the dilation of the entire upper urinary tract.
Prostatic congestion is a medical condition of the prostate gland that happens when the prostate becomes swollen by excess fluid and can be caused by prostatosis. The condition often results in a person with prostatic congestion feeling the urge to urinate frequently. Prostatic congestion has been associated with prostate disease, which can progress due to age. Oftentimes, the prostate will grow in size which can lead to further problems, such as prostatitis, enlarged prostate, or prostate cancer.
Pyelogram is a form of imaging of the renal pelvis and ureter.

Chronic bacterial prostatitis is a bacterial infection of the prostate gland. It should be distinguished from other forms of prostatitis such as acute bacterial prostatitis and chronic pelvic pain syndrome (CPPS).

Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), previously known as chronic nonbacterial prostatitis, is long-term pelvic pain and lower urinary tract symptoms (LUTS) without evidence of a bacterial infection. It affects about 2–6% of men. Together with IC/BPS, it makes up urologic chronic pelvic pain syndrome (UCPPS).

Ureteral cancer is cancer of the ureters, muscular tubes that propel urine from the kidneys to the urinary bladder. It is also known as ureter cancer, renal pelvic cancer, and rarely ureteric cancer or uretal cancer. Cancer in this location is rare. Ureteral cancer becomes more likely in older adults, usually ages 70–80, who have previously been diagnosed with bladder cancer.
References
- 1 2 3 "Kidney Failure". National Institute of Diabetes and Digestive and Kidney Diseases. 2017-10-01. Retrieved 2019-06-17.
- ↑ Baba, T; Murabayashi, S; Tomiyama, T; Takebe, K (1990). "Uncontrolled hypertension is associated with a rapid progression of nephropathy in type 2 diabetic patients with proteinuria and preserved renal function". The Tohoku Journal of Experimental Medicine. 161 (4): 311–8. doi: 10.1620/tjem.161.311 . PMID 2256104.
- ↑ Coresh, Josef; Selvin, Elizabeth; Stevens, Lesley A.; Manzi, Jane; Kusek, John W.; Eggers, Paul; Van Lente, Frederick; Levey, Andrew S. (2007-11-07). "Prevalence of chronic kidney disease in the United States". JAMA. 298 (17): 2038–2047. doi: 10.1001/jama.298.17.2038 . ISSN 1538-3598. PMID 17986697.
- ↑ "What is renal failure?". Johns Hopkins Medicine. Retrieved 18 December 2017.
- ↑ Blakeley, Sara (2010). Renal Failure and Replacement Therapies. Springer Science & Business Media. p. 19. ISBN 9781846289378.
- ↑ Liao, Min-Tser; Sung, Chih-Chien; Hung, Kuo-Chin; Wu, Chia-Chao; Lo, Lan; Lu, Kuo-Cheng (2012). "Insulin Resistance in Patients with Chronic Kidney Disease". Journal of Biomedicine and Biotechnology. 2012: 1–5. doi: 10.1155/2012/691369 . PMC 3420350 . PMID 22919275.
- ↑ "Kidney Failure". MedlinePlus. Retrieved 11 November 2017.
- 1 2 3 "Urinary Tract Infection". CDC. April 17, 2015. Archived from the original on 22 February 2016. Retrieved 9 February 2016.
- 1 2 Lane, DR; Takhar, SS (August 2011). "Diagnosis and management of urinary tract infection and pyelonephritis". Emergency Medicine Clinics of North America. 29 (3): 539–52. doi:10.1016/j.emc.2011.04.001. PMID 21782073.
- ↑ Salvatore S, Salvatore S, Cattoni E, Siesto G, Serati M, Sorice P, Torella M (June 2011). "Urinary tract infections in women". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 156 (2): 131–6. doi:10.1016/j.ejogrb.2011.01.028. PMID 21349630.
- ↑ Woodford, HJ; George, J (February 2011). "Diagnosis and management of urinary infections in older people". Clinical Medicine . 11 (1): 80–3. doi:10.7861/clinmedicine.11-1-80. PMC 5873814 . PMID 21404794.
- 1 2 3 "Interstitial cystitis/bladder pain syndrome fact sheet". OWH. 16 July 2012. Archived from the original on 5 October 2016. Retrieved 6 October 2016.
- ↑ Hanno, PM; Erickson, D; Moldwin, R; Faraday, MM; American Urological, Association (May 2015). "Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment". The Journal of Urology. 193 (5): 1545–53. doi:10.1016/j.juro.2015.01.086. PMID 25623737. Archived from the original on 20 April 2014.
- ↑ Ackley, Betty (2010). Nursing diagnosis handbook : an evidence-based guide to planning care (9th ed.). Maryland Heights, Mo: Mosby. ISBN 9780323071505.
- ↑ Venes, Donald (2013). Taber's cyclopedic medical dictionary. Philadelphia: F.A. Davis. ISBN 9780803629776.
- ↑ "Enuresis". medicaldictionaryweb.com.
- 1 2 "Prostate Enlargement (Benign Prostatic Hyperplasia)". NIDDK. September 2014. Archived from the original on 4 October 2017. Retrieved 19 October 2017.
- ↑ Kim, EH; Larson, JA; Andriole, GL (2016). "Management of Benign Prostatic Hyperplasia". Annual Review of Medicine (Review). 67: 137–51. doi: 10.1146/annurev-med-063014-123902 . PMID 26331999.
- ↑ Kirby, Roger; Carson, Culley C. (January–February 2015). "Editor's Comment on Diagnosis and treatment of chronic prostatitis/chronic pelvic pain syndrome". Trends in Urology and Men's Health. 6 (1): 17. doi: 10.1002/tre.434 .
- ↑ Collins MM, Stafford RS, O'Leary MP, Barry MJ (1998). "How common is prostatitis? A national survey of physician visits". J. Urol. 159 (4): 1224–8. doi:10.1016/S0022-5347(01)63564-X. PMID 9507840.
- 1 2 3 4 5 6 7 8 9 10 "Urinary Retention". National Institute of Diabetes and Digestive and Kidney Diseases. Aug 2014. Archived from the original on 4 October 2017. Retrieved 24 October 2017.
- ↑ Sliwinski, A; D'Arcy, FT; Sultana, R; Lawrentschuk, N (April 2016). "Acute urinary retention and the difficult catheterization: current emergency management". European Journal of Emergency Medicine. 23 (2): 80–8. doi:10.1097/MEJ.0000000000000334. PMID 26479738. S2CID 26988888.
- 1 2 "Bladder Cancer Treatment". National Cancer Institute. 1 January 1980. Archived from the original on 14 July 2017. Retrieved 18 July 2017.
- ↑ "Cancer Fact sheet N°297". World Health Organization. February 2014. Archived from the original on 29 December 2010. Retrieved 10 June 2014.
- ↑ "Defining Cancer". National Cancer Institute. 17 September 2007. Archived from the original on 25 June 2014. Retrieved 10 June 2014.
- ↑ Curti, B; Jana, BRP; Javeed, M; Makhoul, I; Sachdeva, K; Hu, W; Perry, M; Talavera, F (26 February 2014). Harris, JE (ed.). "Renal Cell Carcinoma". Medscape Reference. WebMD. Archived from the original on 7 March 2014. Retrieved 7 March 2014.
- ↑ "Prostate Cancer". National Cancer Institute. January 1980. Archived from the original on 12 October 2014. Retrieved 12 October 2014.
- 1 2 3 4 "Prostate Cancer Treatment (PDQ) – Health Professional Version". National Cancer Institute. 2014-04-11. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- ↑ "Chapter 5.11". World Cancer Report. World Health Organization. 2014. ISBN 978-9283204299.
- ↑ Ruddon, Raymond W. (2007). Cancer biology (4th ed.). Oxford: Oxford University Press. p. 223. ISBN 978-0195175431. Archived from the original on 2015-09-15.
- ↑ "Prostate Cancer Treatment (PDQ) – Patient Version". National Cancer Institute. 2014-04-08. Archived from the original on 5 July 2014. Retrieved 1 July 2014.
- 1 2 Chowdhury SH, Cozma AI, Chowdhury JH. Urinary Tract Obstruction. Essentials for the Canadian Medical Licensing Exam: Review and Prep for MCCQE Part I. 2nd edition. Wolters Kluwer. Hong Kong. 2017.
- 1 2 Gowda S, Desai PB, Kulkarni SS, Hull VV, Math AA, Vernekar SN (2010). "Markers of renal function tests". N Am J Med Sci. 2 (4): 170–3. PMC 3354405 . PMID 22624135.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Po, Henry N.; Senozan, N. M. (2001). "The Henderson-Hasselbalch Equation: Its History and Limitations". Journal of Chemical Education. American Chemical Society (ACS). 78 (11): 1499. Bibcode:2001JChEd..78.1499P. doi:10.1021/ed078p1499. ISSN 0021-9584.
- ↑ Simerville, Jeff A. (2005-03-15). "Urinalysis: A Comprehensive Review". American Family Physician. 71 (6): 1153–1162. ISSN 0002-838X. PMID 15791892 . Retrieved 2019-06-17.
- ↑ Yetisen, Ali Kemal; Akram, Muhammad Safwan; Lowe, Christopher R. (2013-05-21). "Paper-based microfluidic point-of-care diagnostic devices". Lab on a Chip. 13 (12): 2210–2251. doi:10.1039/C3LC50169H. ISSN 1473-0189. PMID 23652632.
- ↑ Rosier, Peter (2019-05-09). "Contemporary diagnosis of lower urinary tract dysfunction". F1000Research. F1000 ( Faculty of 1000 Ltd). 8: 644. doi: 10.12688/f1000research.16120.1 . ISSN 2046-1402. PMC 6509958 . PMID 31119030.
- ↑ American Urogynecologic Society (May 5, 2015), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation , American Urogynecologic Society, retrieved June 1, 2015, which cites: *Gormley, EA; Lightner, DJ; Faraday, M; Vasavada, SP (May 2015). "Diagnosis and Treatment of Overactive Bladder (Non-Neurogenic) in Adults: AUA/SUFU Guideline Amendment". The Journal of Urology. 193 (5): 1572–80. doi:10.1016/j.juro.2015.01.087. PMID 25623739.
- ↑ Piloni, Vittorio Luigi; Spazzafumo, Liana (June 2007). "Sonography of the female pelvic floor:clinical indications and techniques". Pelviperineology. 26 (2): 59–65.
- ↑ Frank, Eugene D.; Long, Bruce W.; Smith, Barbara J. (2012). Merrill's Atlas of Radiographic Positioning & Procedures (12 ed.). St. Louis, MO: Mosby Inc. ISBN 978-0-323-07334-9.
- ↑ Bontrager, Kenneth L.; Lampignano, John P. (2005). Textbook of Radiographic Positioning and Related Anatomy (6 ed.). St. Louis, MO: Mosby, Inc. ISBN 978-0-323-02507-2.
- ↑ Paul Schmitz, MD, et al. Medscape. Kidneys, ureters, and bladder imaging: plain films of the abdomen. Updated 27 Aug 2015.
- ↑ "Intravenous pyelogram". Mayo Clinic. 2018-05-09. Retrieved 2019-06-17.
- ↑ Husband J (2008). Recommendations for Cross-Sectional Imaging in Cancer Management: Computed Tomography – CT Magnetic Resonance Imaging – MRI Positron Emission Tomography – PET-CT (PDF). Royal College of Radiologists. ISBN 978-1-905034-13-0.
- ↑ Frimberger, Dominic; Bauer, Stuart B.; Cain, Mark P.; Greenfield, Saul P.; Kirsch, Andrew J.; Ramji, Faridali; Mercado-Deane, Maria-Gisela; Cooper, Christoper S. (2016-12-01). "Establishing a standard protocol for the voiding cystourethrography". Journal of Pediatric Urology. 12 (6): 362–366. doi:10.1016/j.jpurol.2016.11.001. ISSN 1477-5131. PMID 27939178. S2CID 21041368.