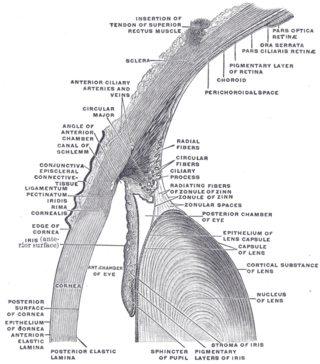
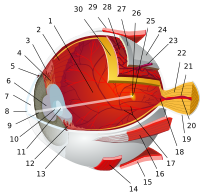
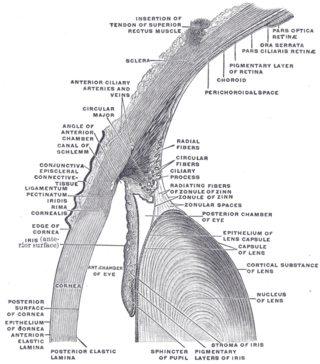
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

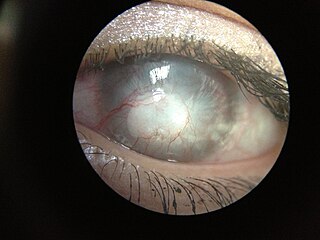
A pterygium of the eye is a pinkish, roughly triangular tissue growth of the conjunctiva onto the cornea of the eye. It typically starts on the cornea near the nose. It may slowly grow but rarely grows so large that it covers the pupil and impairs vision. Often both eyes are involved.

Eye surgery, also known as ophthalmic surgery or ocular surgery, is surgery performed on the eye or its adnexa. Eye surgery is part of ophthalmology and is performed by an ophthalmologist or eye surgeon. The eye is a fragile organ, and requires due care before, during, and after a surgical procedure to minimize or prevent further damage. An eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. It continues to be a widely practiced class of surgery, with various techniques having been developed for treating eye problems.

Refractive surgery is optional eye surgery used to improve the refractive state of the eye and decrease or eliminate dependency on glasses or contact lenses. This can include various methods of surgical remodeling of the cornea (keratomileusis), lens implantation or lens replacement. The most common methods today use excimer lasers to reshape the curvature of the cornea. Refractive eye surgeries are used to treat common vision disorders such as myopia, hyperopia, presbyopia and astigmatism.
In the anatomy of the eye, the conjunctiva is a thin mucous membrane that lines the inside of the eyelids and covers the sclera. It is composed of non-keratinized, stratified squamous epithelium with goblet cells, stratified columnar epithelium and stratified cuboidal epithelium. The conjunctiva is highly vascularised, with many microvessels easily accessible for imaging studies.

A phakic intraocular lens (PIOL) is an intraocular lens that is implanted surgically into the eye to correct refractive errors without removing the natural lens. Intraocular lenses that are implanted into eyes after the eye's natural lens has been removed during cataract surgery are known as pseudophakic.

A red eye is an eye that appears red due to illness or injury. It is usually injection and prominence of the superficial blood vessels of the conjunctiva, which may be caused by disorders of these or adjacent structures. Conjunctivitis and subconjunctival hemorrhage are two of the less serious but more common causes.

Hyphema is the medical condition of bleeding in the anterior chamber of the eye between the iris and the cornea. People usually first notice a loss or decrease in vision. The eye may also appear to have a reddish tinge, or it may appear as a small pool of blood at the bottom of the iris in the cornea. A traumatic hyphema is caused by a blow to the eye. A hyphema can also occur spontaneously.
Ocular melanosis (OM) is a blue-gray and/or brown lesion of the conjunctiva that can be separated into benign conjunctival epithelial melanosis (BCEM) and primary acquired melanosis (PAM), of which the latter is considered a risk factor for uveal melanoma. The disease is caused by an increase of melanocytes in the iris, choroid, and surrounding structures. Overproduction of pigment by these cells can block the trabecular meshwork through which fluid drains from the eye. The increased fluid in the eye leads to increased pressure, which can lead to glaucoma. In humans, this is sometimes known as pigment dispersion syndrome.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.

Vernal keratoconjunctivitis is a recurrent, bilateral, and self-limiting type of conjunctivitis having a periodic seasonal incidence.

A pinguecula is a common type of conjunctival stromal degeneration in the eye. It appears as an elevated yellow-white plaque in the bulbar conjunctiva near the limbus. Calcification may also seen occasionally.
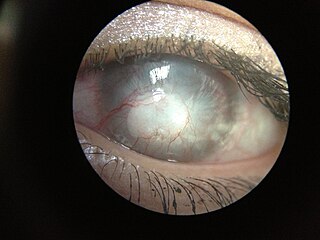
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of healthy corneal physiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.

Corneal ulcer, also called keratitis, is an inflammatory or, more seriously, infective condition of the cornea involving disruption of its epithelial layer with involvement of the corneal stroma. It is a common condition in humans particularly in the tropics and in farming. In developing countries, children afflicted by vitamin A deficiency are at high risk for corneal ulcer and may become blind in both eyes persisting throughout life. In ophthalmology, a corneal ulcer usually refers to having an infection, while the term corneal abrasion refers more to a scratch injury.
A staphyloma is an abnormal protrusion of the uveal tissue through a weak point in the eyeball. The protrusion is generally black in colour, due to the inner layers of the eye. It occurs due to weakening of outer layer of eye by an inflammatory or degenerative condition. It may be of five types, depending on the location on the eyeball.

A limbal ring is a dark ring around the iris of the eye, where the sclera meets the cornea. It is a dark-colored manifestation of the corneal limbus resulting from optical properties of the region. The appearance and visibility of the limbal ring can be negatively affected by a variety of medical conditions concerning the peripheral cornea. It has been suggested that limbal ring thickness may correlate with health or youthfulness and may contribute to facial attractiveness. The thickness of the limbal ring varies by pupil dilation - when the pupil is larger, the limbal ring narrows. Some contact lenses are colored to simulate limbal rings.
Open-globe injuries are full-thickness eye-wall wounds requiring urgent diagnosis and treatment.

Limbal stem cells, also known as corneal epithelial stem cells, are unipotent stem cells located in the basal epithelial layer of the corneal limbus. They form the border between the cornea and the sclera. Characteristics of limbal stem cells include a slow turnover rate, high proliferative potential, clonogenicity, expression of stem cell markers, as well as the ability to regenerate the entire corneal epithelium. Limbal stem cell proliferation has the role of maintaining the cornea; for example, by replacing cells that are lost via tears. Additionally, these cells also prevent the conjunctival epithelial cells from migrating onto the surface of the cornea.
An artificial iris is an intraocular implant that is used as both a cosmetic and to treat those with aniridia or other eye trauma. People with this condition experience photophobia, or increased sensitivity to light. The artificial iris, made from silicone, acts as a replacement iris. The artificial iris is implanted in the eye using different surgery techniques depending on the patient's eye trauma. Most of the major artificial iris manufacturers are European and the treatment is used sparingly in the United States because of limited FDA approval, in part due to possibility of vision loss and other risks.
Manual small incision cataract surgery (MSICS) is an evolution of extracapsular cataract extraction (ECCE); the lens is removed from the eye through a self-sealing scleral tunnel wound. A well-constructed scleral tunnel is held closed by internal pressure, is watertight, and does not require suturing. The wound is relatively smaller than that in ECCE but is still markedly larger than a phacoemulsification wound. Comparative trials of MSICS against phaco in dense cataracts have found no statistically significant difference in outcomes but MSICS had shorter operating times and significantly lower costs. MSICS has become the method of choice in the developing world because it provides high-quality outcomes with less surgically induced astigmatism than ECCE, no suture-related problems, quick rehabilitation, and fewer post-operative visits. MSICS is easy and fast to learn for the surgeon, cost effective, simple, and applicable to almost all types of cataract.