A tendon or sinew is a tough band of dense fibrous connective tissue that connects muscle to bone. It sends the mechanical forces of muscle contraction to the skeletal system, while withstanding tension.

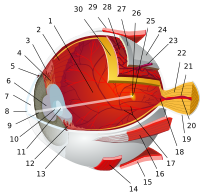
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

The Bowman's layer is a smooth, acellular, nonregenerating layer, located between the superficial epithelium and the stroma in the cornea of the eye. It is composed of strong, randomly oriented collagen fibrils in which the smooth anterior surface faces the epithelial basement membrane and the posterior surface merges with the collagen lamellae of the corneal stroma proper.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.
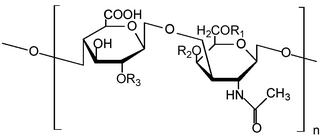
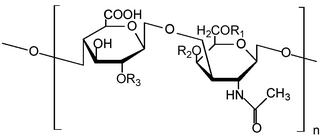
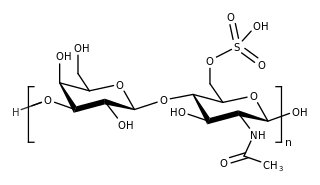
Glycosaminoglycans (GAGs) or mucopolysaccharides are long, linear polysaccharides consisting of repeating disaccharide units. The repeating two-sugar unit consists of a uronic sugar and an amino sugar, except in the case of the sulfated glycosaminoglycan keratan, where, in place of the uronic sugar there is a galactose unit. GAGs are found in vertebrates, invertebrates and bacteria. Because GAGs are highly polar molecules and attract water; the body uses them as lubricants or shock absorbers.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.
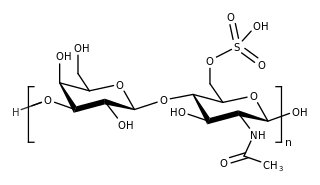
Keratan sulfate (KS), also called keratosulfate, is any of several sulfated glycosaminoglycans that have been found especially in the cornea, cartilage, and bone. It is also synthesized in the central nervous system where it participates both in development and in the glial scar formation following an injury. Keratan sulfates are large, highly hydrated molecules which in joints can act as a cushion to absorb mechanical shock.

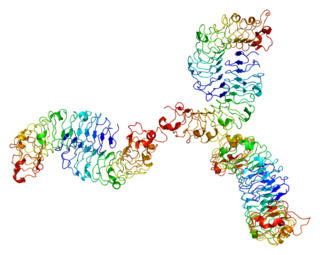
Decorin is a protein that in humans is encoded by the DCN gene.
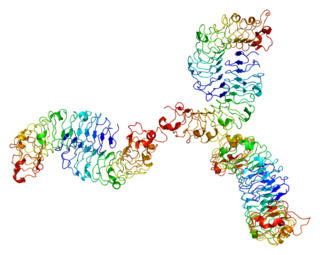
Biglycan is a small leucine-rich repeat proteoglycan (SLRP) which is found in a variety of extracellular matrix tissues, including bone, cartilage and tendon. In humans, biglycan is encoded by the BGN gene which is located on the X chromosome.

Pellucid marginal degeneration (PMD) is a degenerative corneal condition, often confused with keratoconus. It typically presents with painless vision loss affecting both eyes. Rarely, it may cause acute vision loss with severe pain due to perforation of the cornea. It is typically characterized by a clear, bilateral thinning (ectasia) in the inferior and peripheral region of the cornea, although some cases affect only one eye. The cause of the disease remains unclear.

Lumican, also known as LUM, is an extracellular matrix protein that, in humans, is encoded by the LUM gene on chromosome 12.

Keratocan (KTN) also known as keratan sulfate proteoglycan keratocan, is a protein that in humans is encoded by the KERA gene.

Dermatopontin also known as tyrosine-rich acidic matrix protein (TRAMP) is a protein that in humans is encoded by the DPT gene. Dermatopontin is a 22-kDa protein of the noncollagenous extracellular matrix (ECM) estimated to comprise 12 mg/kg of wet dermis weight. To date, homologues have been identified in five different mammals and 12 different invertebrates with multiple functions. In vertebrates, the primary function of dermatopontin is a structural component of the ECM, cell adhesion, modulation of TGF-β activity and cellular quiescence). It also has pathological involvement in heart attacks and decreased expression in leiomyoma and fibrosis. In invertebrate, dermatopontin homologue plays a role in hemagglutination, cell-cell aggregation, and expression during parasite infection.

The ocular immune system protects the eye from infection and regulates healing processes following injuries. The interior of the eye lacks lymph vessels but is highly vascularized, and many immune cells reside in the uvea, including mostly macrophages, dendritic cells, and mast cells. These cells fight off intraocular infections, and intraocular inflammation can manifest as uveitis or retinitis. The cornea of the eye is immunologically a very special tissue. Its constant exposure to the exterior world means that it is vulnerable to a wide range of microorganisms while its moist mucosal surface makes the cornea particularly susceptible to attack. At the same time, its lack of vasculature and relative immune separation from the rest of the body makes immune defense difficult. Lastly, the cornea is a multifunctional tissue. It provides a large part of the eye's refractive power, meaning it has to maintain remarkable transparency, but must also serve as a barrier to keep pathogens from reaching the rest of the eye, similar to function of the dermis and epidermis in keeping underlying tissues protected. Immune reactions within the cornea come from surrounding vascularized tissues as well as innate immune responsive cells that reside within the cornea.

Macular corneal dystrophy, also known as Fehr corneal dystrophy, is a rare pathological condition affecting the stroma of cornea first described by Arthur Groenouw in 1890. Signs are usually noticed in the first decade of life and progress afterwards, with opacities developing in the cornea and attacks of pain. This gradual opacification leads to visual impairment often requiring keratoplasty in the later decades of life.
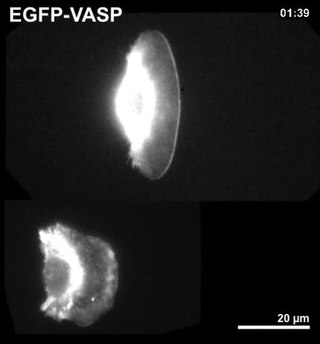
Corneal keratocytes are specialized fibroblasts residing in the stroma. This corneal layer, representing about 85-90% of corneal thickness, is built up from highly regular collagenous lamellae and extracellular matrix components. Keratocytes play the major role in keeping it transparent, healing its wounds, and synthesizing its components. In the unperturbed cornea keratocytes stay dormant, coming into action after any kind of injury or inflammation. Some keratocytes underlying the site of injury, even a light one, undergo apoptosis immediately after the injury. Any glitch in the precisely orchestrated process of healing may cloud the cornea, while excessive keratocyte apoptosis may be a part of the pathological process in the degenerative corneal disorders such as keratoconus, and these considerations prompt the ongoing research into the function of these cells.

Congenital stromal corneal dystrophy (CSCD) is an extremely rare, autosomal dominant form of corneal dystrophy. Only 4 families have been reported to have the disease by 2009. The main features of the disease are numerous opaque flaky or feathery areas of clouding in the stroma that multiply with age and eventually preclude visibility of the endothelium. Strabismus or primary open angle glaucoma was noted in some of the patients. Thickness of the cornea stays the same, Descemet's membrane and endothelium are relatively unaffected, but the fibrils of collagen that constitute stromal lamellae are reduced in diameter and lamellae themselves are packed significantly more tightly.

Sclerocornea is a congenital anomaly of the eye in which the cornea blends with sclera, having no clear-cut boundary. The extent of the resulting opacity varies from peripheral to total. The severe form is thought to be inherited in an autosomal recessive manner, but there may be another, milder form that is expressed in a dominant fashion. In some cases the patients also have abnormalities beyond the eye (systemic), such as limb deformities and craniofacial and genitourinary defects.
In crystallography, short range order refers to the regular and predictable arrangement of atoms over a short distance, usually with one or two atom spacings. However, this regularity described by short-range order does not necessarily apply to a larger area. Examples of materials with short range order include amorphous materials such as wax, glass and liquids as well as the collagen fibrils of the stroma in the cornea.

The human cornea is a transparent membrane which allows light to pass through it. The word corneal opacification literally means loss of normal transparency of cornea. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term corneal blindness is commonly used to describe blindness due to corneal opacity.