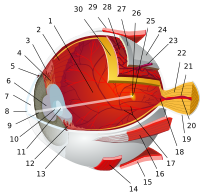
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

Laser-Assisted in Situ Keratomileusis (LASIK), commonly referred to as laser eye surgery or laser vision correction, is a type of refractive surgery for the correction of myopia, hyperopia, and an actual cure for astigmatism, since it is in the cornea. LASIK surgery is performed by an ophthalmologist who uses a laser or microkeratome to reshape the eye's cornea in order to improve visual acuity.

Photorefractive keratectomy (PRK) and laser-assisted sub-epithelial keratectomy (LASEK) are laser eye surgery procedures intended to correct a person's vision, reducing dependency on glasses or contact lenses. LASEK and PRK permanently change the shape of the anterior central cornea using an excimer laser to ablate a small amount of tissue from the corneal stroma at the front of the eye, just under the corneal epithelium. The outer layer of the cornea is removed prior to the ablation.
A microkeratome is a precision surgical instrument with an oscillating blade designed for creating the corneal flap in LASIK or ALK surgery. The normal human cornea varies from around 500 to 600 μm in thickness; and in the LASIK procedure, the microkeratome creates an 83 to 200 μm thick flap. The microkeratome uses an oscillating blade system, which has a blade that oscillates horizontally as the blade travels vertically for a precise cut. This piece of equipment is used all around the world to cut the cornea flap. The microkeratome is also used in Descemet's stripping automated endothelial keratoplasty (DSAEK), where it is used to slice a thin layer from the back of the donor cornea, which is then transplanted into the posterior cornea of the recipient. It was invented by Jose Barraquer and Cesar Carlos Carriazo in the 1950s in Colombia.

Radial keratotomy (RK) is a refractive surgical procedure to correct myopia (nearsightedness). It was developed in 1974 by Svyatoslav Fyodorov, a Russian ophthalmologist. It has been largely supplanted by newer, more accurate operations, such as photorefractive keratectomy, LASIK, Epi-LASIK and the phakic intraocular lens.

Refractive surgery is optional eye surgery used to improve the refractive state of the eye and decrease or eliminate dependency on glasses or contact lenses. This can include various methods of surgical remodeling of the cornea (keratomileusis), lens implantation or lens replacement. The most common methods today use excimer lasers to reshape the curvature of the cornea. Refractive eye surgeries are used to treat common vision disorders such as myopia, hyperopia, presbyopia and astigmatism.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.
Epi-LASIK is a refractive surgery technique designed to reduce a person's dependency on eyeglasses and contact lenses. Invented by Dr. Ioannis Pallikaris, the technique is basically an automatic LASEK without alcohol; it can be better considered as superficial LASIK. The stromal bed is smoother than that obtained by mechanical methods or brush. Unlike alcohol (LASEK), there is no chance of damaging the limbal stem cells. It is also relatively less painful than LASEK.
- A device similar to a microkeratome slides over the surface of the cornea, just underneath the epithelial layer of cells while suction is applied.
- The result is a hinged sheet of epithelium that is at least partially viable.
- It is reflected out of the way so that the ablation can take place.
- The sheet is repositioned and a bandage soft contact lens is placed on the eye.

Fuchs dystrophy, also referred to as Fuchs endothelial corneal dystrophy (FECD) and Fuchs endothelial dystrophy (FED), is a slowly progressing corneal dystrophy that usually affects both eyes and is slightly more common in women than in men. Although early signs of Fuchs dystrophy are sometimes seen in people in their 30s and 40s, the disease rarely affects vision until people reach their 50s and 60s.

Recurrent corneal erosion is a disorder of the eyes characterized by the failure of the cornea's outermost layer of epithelial cells to attach to the underlying basement membrane. The condition is excruciatingly painful because the loss of these cells results in the exposure of sensitive corneal nerves. This condition can often leave patients with temporary blindness due to extreme light sensitivity (photophobia).

Corneal cross-linking (CXL) with riboflavin (vitamin B2) and UV-A light is a surgical treatment for corneal ectasia such as keratoconus, PMD, and post-LASIK ectasia.

Descemet's membrane is the basement membrane that lies between the corneal proper substance, also called stroma, and the endothelial layer of the cornea. It is composed of different kinds of collagen than the stroma. The endothelial layer is located at the posterior of the cornea. Descemet's membrane, as the basement membrane for the endothelial layer, is secreted by the single layer of squamous epithelial cells that compose the endothelial layer of the cornea.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.

Corneal ulcer, also called keratitis, is an inflammatory or, more seriously, infective condition of the cornea involving disruption of its epithelial layer with involvement of the corneal stroma. It is a common condition in humans particularly in the tropics and in farming. In developing countries, children afflicted by vitamin A deficiency are at high risk for corneal ulcer and may become blind in both eyes persisting throughout life. In ophthalmology, a corneal ulcer usually refers to having an infection, while the term corneal abrasion refers more to a scratch injury.

Meesmann corneal dystrophy (MECD) is a rare hereditary autosomal dominant disease that is characterized as a type of corneal dystrophy and a keratin disease. MECD is characterized by the formation of microcysts in the outermost layer of the cornea, known as the anterior corneal epithelium. The anterior corneal epithelium also becomes fragile. This usually affects both eyes rather than a single eye and worsens over time. There are two phenotypes, Meesmann corneal dystrophy 1 (MECD1) and Meesmann corneal dystrophy 2 (MECD2), which affect the genes KRT3 and KRT12, respectively. A heterozygous mutation in either of these genes will lead to a single phenotype. Many with Meesmann corneal dystrophy are asymptomatic or experience mild symptoms.
Diffuse lamellar keratitis (DLK) is a sterile inflammation of the cornea which may occur after refractive surgery, such as LASIK. Its incidence has been estimated to be 1 in 500 patients, though this may be as high as 32% in some cases.
Peter S. Hersh is an American ophthalmologist and specialist in LASIK eye surgery, keratoconus, and diseases of the cornea. He co-authored the article in the journal Ophthalmology that presented the results of the study that led to the first approval by the U.S. Food and Drug Administration (FDA) of the excimer laser for the correction of nearsightedness in the United States. Hersh was also medical monitor of the study that led to approval of corneal collagen crosslinking for the treatment of keratoconus.
Post-LASIK ectasia is a condition similar to keratoconus where the cornea starts to bulge forwards at a variable time after LASIK, PRK, or SMILE corneal laser eye surgery. However, the physiological processes of post-LASIK ectasia seem to be different from keratoconus. The visible changes in the basal epithelial cell and anterior and posterior keratocytes linked with keratoconus were not observed in post-LASIK ectasia.

Limbal stem cells, also known as corneal epithelial stem cells, are unipotent stem cells located in the basal epithelial layer of the corneal limbus. They form the border between the cornea and the sclera. Characteristics of limbal stem cells include a slow turnover rate, high proliferative potential, clonogenicity, expression of stem cell markers, as well as the ability to regenerate the entire corneal epithelium. Limbal stem cell proliferation has the role of maintaining the cornea; for example, by replacing cells that are lost via tears. Additionally, these cells also prevent the conjunctival epithelial cells from migrating onto the surface of the cornea.
Pre Descemet's endothelial keratoplasty (PDEK) is a kind of endothelial keratoplasty, where the pre descemet's layer (PDL) along with descemet's membrane (DM) and endothelium is transplanted. Conventionally in a corneal transplantation, doctors use a whole cornea or parts of the five layers of the cornea to perform correction surgeries. In May 2013, Dr Harminder Dua discovered a sixth layer between the stroma and the descemet membrane which was named after him as the Dua's layer. In the PDEK technique, doctors take the innermost two layers of the cornea, along with the Dua's layer and graft it in the patient's eye.