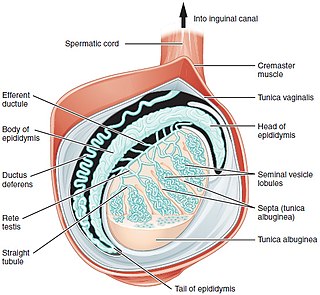
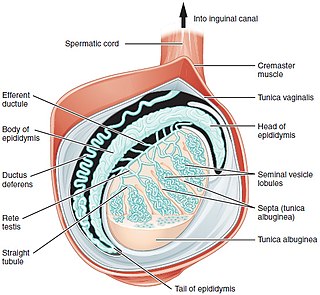
Testicular torsion occurs when the spermatic cord twists, cutting off the blood supply to the testicle. The most common symptom in children is sudden, severe testicular pain. The testicle may be higher than usual in the scrotum and vomiting may occur. In newborns, pain is often absent and instead the scrotum may become discolored or the testicle may disappear from its usual place.

Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle or swelling or pain in the scrotum. Treatment may result in infertility.

Cryptorchidism, also known as undescended testis, is the failure of one or both testes to descend into the scrotum. The word is from Greek κρυπτός 'hidden' and ὄρχις 'testicle'. It is the most common birth defect of the male genital tract. About 3% of full-term and 30% of premature infant boys are born with at least one undescended testis. However, about 80% of cryptorchid testes descend by the first year of life, making the true incidence of cryptorchidism around 1% overall. Cryptorchidism may develop after infancy, sometimes as late as young adulthood, but that is exceptional.

Epididymal hypertension (EH), informally referred to as blue balls for men or blue vulva for women, is a harmless but uncomfortable sensation in the genital regions during a prolonged state of sexual arousal. It usually resolves within hours unless relieved through an orgasm.

Orchiopexy is a surgery to move and/or permanently fix a testicle into the scrotum. While orchiopexy typically describes the operation to surgically correct an undescended testicle, it is also used to resolve testicular torsion.

Spermatocele is a fluid-filled cyst that develops in the epididymis. The fluid is usually a clear or milky white color and may contain sperm. Spermatoceles are typically filled with spermatozoa and they can vary in size from several millimeters to many centimeters. Small spermatoceles are relatively common, occurring in an estimated 30 percent of males. They are generally not painful. However, some people may experience discomfort such as a dull pain in the scrotum from larger spermatoceles. They are not cancerous, nor do they cause an increased risk of testicular cancer. Additionally, unlike varicoceles, they do not reduce fertility.

Testicular atrophy is a medical condition in which one or both testicles diminish in size and may be accompanied by reduced testicular function. Testicular atrophy is not related to the temporary shrinkage of the surrounding scrotum, which might occur in response to cold temperature.

A varicocele is, in a male person, an abnormal enlargement of the pampiniform venous plexus in the scrotum; in a female person, it is an abnormal painful swelling to the embryologically identical pampiniform venous plexus; it is more commonly called pelvic compression syndrome. In the male varicocele, this plexus of veins drains blood from the testicles back to the heart. The vessels originate in the abdomen and course down through the inguinal canal as part of the spermatic cord on their way to the testis. Varicoceles occur in around 15% to 20% of all men. The incidence of varicocele increase with age.

Anogenital distance (AGD) is the distance from the midpoint of the anus to the genitalia, the underside of the vagina, the clitoris or the scrotum. It is considered medically significant for a number of reasons, in both humans and other animals, including sex determination and as a marker of endocrine disruptor exposure. It is regulated by dihydrotestosterone, which can be disrupted by phthalates common in plastics.
Male infertility refers to a sexually mature male's inability to impregnate a fertile female. In humans it accounts for 40–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. More recently, advance sperm analyses that examine intracellular sperm components are being developed.

Testicular pain, also known as scrotal pain, occurs when part or all of either one or both testicles hurt. Pain in the scrotum is also often included. Testicular pain may be of sudden onset or of long duration.

Gonadal dysgenesis is classified as any congenital developmental disorder of the reproductive system in humans. It is atypical development of gonads in an embryo,. One type of gonadal dysgenesis is the development of functionless, fibrous tissue, termed streak gonads, instead of reproductive tissue. Streak gonads are a form of aplasia, resulting in hormonal failure that manifests as sexual infantism and infertility, with no initiation of puberty and secondary sex characteristics.
Testicular sperm extraction (TESE) is a surgical procedure in which a small portion of tissue is removed from the testicle and any viable sperm cells from that tissue are extracted for use in further procedures, most commonly intracytoplasmic sperm injection (ICSI) as part of in vitro fertilisation (IVF). TESE is often recommended to patients who cannot produce sperm by ejaculation due to azoospermia.
Post-vasectomy pain syndrome (PVPS) is a chronic and sometimes debilitating genital pain condition that may develop immediately or several years after vasectomy. Because this condition is a syndrome, there is no single treatment method, therefore efforts focus on mitigating/relieving the individual patient's specific pain. When pain in the epididymides is the primary symptom, post-vasectomy pain syndrome is often described as congestive epididymitis.

A micropenis is an unusually small penis. A common criterion is a dorsal penile length of at least 2.5 standard deviations smaller than the mean human penis size. A micropenis is stretched penile length less than 2.5 cm in term infants, 2.6 cm in one-year-old, 3.5 cm in five year old, 3.8 cm in ten year old, and 9.3 cm in adults. The condition is usually recognized shortly after birth. The term is most often used medically when the rest of the penis, scrotum, and perineum are without ambiguity, such as hypospadias. A microphallus describes a medical term where other sections of genitallia are different, such as hypospadias or cryptorchidism. Micropenis incidence is about 1.5 in 10,000 male newborns in North America.

Orchiectomy is a surgical procedure in which one or both testicles are removed. The surgery can be performed for various reasons:

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Ectopic testis is used to describe the testis leaving the inguinal canal and entering a site other than the scrotum. Usually, it results from obstruction of the scrotal entrance or from overdevelopment and lengthening of a segment of the gubernaculum.
Male genital examination is a physical examination of the genital in males to detect ailments and to assess sexual development, and is normally a component of an annual physical examination. The examination includes checking the penis, scrotum, and urethral meatus. A comprehensive assessment of the male genitals assesses the pubic hair based on Sexual Maturity Rating and the size of the testicles and penis. The exam can also be conducted to verify a person's age and biological sex. The genitourinary system can also be assessed as part of the male genital examination. During a genital examination, the doctor can detect any of the following: structural abnormalities, urethral opening abnormalities, problems related to not being circumcised, lumps, tumors, redness, excoriation, edema, lesions, swelling, cancer, hair-related issues, and many others. In some instances where a physical examination of the male genitals is not sufficient to diagnose an individual, then an internal genital examination using imaging or ultrasounds will be needed for further evaluation.
Testicular dysgenesis syndrome is a male reproduction-related condition characterized by the presence of symptoms and disorders such as hypospadias, cryptorchidism, poor semen quality, and testicular cancer. The concept was first introduced by N.E. Skakkaebaek in a research paper along with the department of Growth and Reproduction in Copenhagen University. The paper suggests the origin and underlying cause of TDS can be detected as early as in fetal life, where environmental and genomic factors could affect the development of the male reproductive system.