Loa loa filariasis, (Loiasis) is a skin and eye disease caused by the nematode worm Loa loa. Humans contract this disease through the bite of a deer fly or mango fly, the vectors for Loa loa. The adult Loa loa filarial worm migrates throughout the subcutaneous tissues of humans, occasionally crossing into subconjunctival tissues of the eye where it can be easily observed. Loa loa does not normally affect vision but can be painful when moving about the eyeball or across the bridge of the nose. Loiasis can cause red itchy swellings below the skin called "Calabar swellings". The disease is treated with the drug diethylcarbamazine (DEC), and when appropriate, surgical methods may be employed to remove adult worms from the conjunctiva. Loiasis belongs to the group of neglected tropical diseases.

Loa loa is a filarial (arthropod-borne) nematode (roundworm) that causes Loa loa filariasis. Loa loa actually means "worm worm", but is commonly known as the "eye worm", as it localizes to the conjunctiva of the eye. Loa loa is commonly found in Africa. It mainly inhabits rain forests in West Africa and has native origins in Ethiopia. The disease caused by Loa loa is called loiasis and is one of the neglected tropical diseases.

Diethylcarbamazine is a medication used in the treatment of filariasis including lymphatic filariasis, tropical pulmonary eosinophilia, and loiasis. It may also be used for prevention of loiasis in those at high risk. While it has been used for onchocerciasis, ivermectin is preferred. It is taken by mouth.

Onchocerciasis, also known as river blindness, is a disease caused by infection with the parasitic worm Onchocerca volvulus. Symptoms include severe itching, bumps under the skin, and blindness. It is the second-most common cause of blindness due to infection, after trachoma.

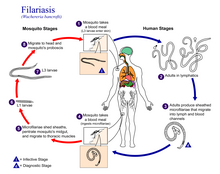
Wuchereria bancrofti is a filarial (arthropod-borne) nematode (roundworm) that is the major cause of lymphatic filariasis. It is one of the three parasitic worms, together with Brugia malayi and B. timori, that infect the lymphatic system to cause lymphatic filariasis. These filarial worms are spread by a variety of mosquito vector species. W. bancrofti is the most prevalent of the three and affects over 120 million people, primarily in Central Africa and the Nile delta, South and Central America, the tropical regions of Asia including southern China, and the Pacific islands. If left untreated, the infection can develop into lymphatic filariasis. In rare conditions, it also causes tropical pulmonary eosinophilia. No vaccine is commercially available, but high rates of cure have been achieved with various antifilarial regimens, and lymphatic filariasis is the target of the World Health Organization Global Program to Eliminate Lymphatic Filariasis with the aim to eradicate the disease as a public-health problem by 2020. However, this goal was not met by 2020.

Brugia malayi is a filarial (arthropod-borne) nematode (roundworm), one of the three causative agents of lymphatic filariasis in humans. Lymphatic filariasis, also known as elephantiasis, is a condition characterized by swelling of the lower limbs. The two other filarial causes of lymphatic filariasis are Wuchereria bancrofti and Brugia timori, which both differ from B. malayi morphologically, symptomatically, and in geographical extent.

Onchocerca volvulus is a filarial (arthropod-borne) nematode (roundworm) that causes onchocerciasis, and is the second-leading cause of blindness due to infection worldwide after trachoma. It is one of the 20 neglected tropical diseases listed by the World Health Organization, with elimination from certain countries expected by 2025.
Brugia pahangi is a parasitic roundworm belonging to the genus Brugia. It is a filarial nematode known to infect the lymph vessels of domestic cats and wild animals, causing a disease filariasis.

Lymphatic filariasis is a human disease caused by parasitic worms known as filarial worms. Usually acquired in childhood, it is a leading cause of permanent disability worldwide, impacting over a hundred million people and manifesting itself in a variety of severe clinical pathologies While most cases have no symptoms, some people develop a syndrome called elephantiasis, which is marked by severe swelling in the arms, legs, breasts, or genitals. The skin may become thicker as well, and the condition may become painful. Affected people are often unable to work and are often shunned or rejected by others because of their disfigurement and disability.
In population ecology, density-dependent processes occur when population growth rates are regulated by the density of a population. This article will focus on density dependence in the context of macroparasite life cycles.

Mansonella perstans is a filarial (arthropod-borne) nematode (roundworm), transmitted by tiny blood-sucking flies called midges. Mansonella perstans is one of two filarial nematodes that causes serous cavity filariasis in humans. The other filarial nematode is Mansonella ozzardi. M. perstans is widespread in many parts of sub-Saharan Africa, parts of Central and South America, and the Caribbean.
Mansonelliasis is the condition of infection by the nematode Mansonella. The disease exists in Africa and tropical Americas, spread by biting midges or blackflies. It is usually asymptomatic.
Brugia timori is a filarial (arthropod-borne) nematode (roundworm) which causes the disease "Timor filariasis", or "Timorian filariasis". While this disease was first described in 1965, the identity of Brugia timori as the causative agent was not known until 1977. In that same year, Anopheles barbirostris was shown to be its primary vector. There is no known animal reservoir host.

The Onchocercidae are a family of nematodes in the superfamily Filarioidea. This family includes some of the most devastating human parasitic diseases, such as lymphatic filariasis, onchocerciasis, loiasis, and other filariases.
Mansonella ozzardi is a filarial (arthropod-borne) nematode (roundworm). This filarial nematode is one of two that causes serous cavity filariasis in humans. The other filarial nematode that causes it in humans is Mansonella perstans. M. ozzardi is an endoparasite that inhabits the serous cavity of the abdomen in the human host. It lives within the mesenteries, peritoneum, and in the subcutaneous tissue.

The Filarioidea are a superfamily of highly specialised parasitic nematodes. Species within this superfamily are known as filarial worms or filariae. Infections with parasitic filarial worms cause disease conditions generically known as filariasis. Drugs against these worms are known as filaricides.
Mansonella streptocerca,, is a filarial (arthropod-borne) nematode (roundworm) causing the disease streptocerciasis. It is a common parasite in the skin of humans in the rain forests of Africa, where it is thought to be a parasite of chimpanzees, as well.
Tropical pulmonary eosinophilia, is characterized by cough, bronchospasm, wheezing, abdominal pain, and an enlarged spleen. Occurring most frequently in the Indian subcontinent and Southeast Asia, TPE is a clinical manifestation of lymphatic filariasis, a parasitic infection caused by filarial roundworms that inhabit the lymphatic vessels, lymph nodes, spleen, and bloodstream. Three species of filarial roundworms, all from the Onchocercidae family, cause human lymphatic filariasis: Wuchereria bancrofti, Brugia malayi, and Brugia timori.

Brugia is a genus for a group of small roundworms. They are among roundworms that cause the parasitic disease filariasis. Specifically, of the three species known, Brugia malayi and Brugia timori cause lymphatic filariasis in humans; and Brugia pahangi and Brugia patei infect domestic cats, dogs and other animals. They are transmitted by the bite of mosquitos.
Lymphatic filariasis in India refers to the presence of the disease lymphatic filariasis in India and the social response to the disease. In India, 99% of infections come from a type of mosquito spreading a type of worm through a mosquito bite. The treatment plan provides 400 million people in India with medication to eliminate the parasite. About 50 million people in India were carrying the worm as of the early 2010s, which is 40% of all the cases in the world. In collaboration with other countries around the world, India is participating in a global effort to eradicate lymphatic filariasis. If the worm is eliminated from India then the disease could be permanently eradicated. In October 2019 the Union health minister Harsh Vardhan said that India's current plan is on schedule to eradicate filariasis by 2021.