Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The process of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.

Prothrombin is encoded in the human by the F2 gene. It is proteolytically cleaved during the clotting process by the prothrombinase enzyme complex to form thrombin.

Antithrombin (AT) is a small glycoprotein that inactivates several enzymes of the coagulation system. It is a 464-amino-acid protein produced by the liver. It contains three disulfide bonds and a total of four possible glycosylation sites. α-Antithrombin is the dominant form of antithrombin found in blood plasma and has an oligosaccharide occupying each of its four glycosylation sites. A single glycosylation site remains consistently un-occupied in the minor form of antithrombin, β-antithrombin. Its activity is increased manyfold by the anticoagulant drug heparin, which enhances the binding of antithrombin to factor IIa (thrombin) and factor Xa.

Von Willebrand factor (VWF) is a blood glycoprotein that promotes hemostasis, specifically, platelet adhesion. It is deficient and/or defective in von Willebrand disease and is involved in many other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic–uremic syndrome. Increased plasma levels in many cardiovascular, neoplastic, metabolic, and connective tissue diseases are presumed to arise from adverse changes to the endothelium, and may predict an increased risk of thrombosis.

Plasmin is an important enzyme present in blood that degrades many blood plasma proteins, including fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein is encoded by the PLG gene.
High-molecular-weight kininogen is a circulating plasma protein which participates in the initiation of blood coagulation, and in the generation of the vasodilator bradykinin via the kallikrein-kinin system. HMWK is inactive until it either adheres to binding proteins beneath an endothelium disrupted by injury, thereby initiating coagulation; or it binds to intact endothelial cells or platelets for functions other than coagulation.

Coagulation factor VII is a protein involved in coagulation and, in humans, is encoded by gene F7. It is an enzyme of the serine protease class. Once bound to tissue factor released from damaged tissues, it is converted to factor VIIa, which in turn activates factor IX and factor X.

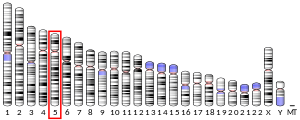
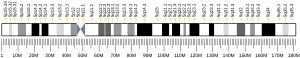
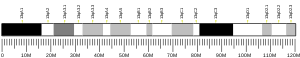
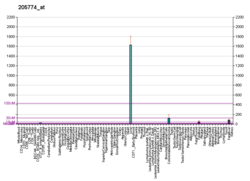
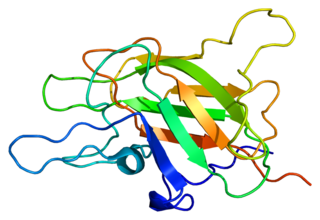
Protein C, also known as autoprothrombin IIA and blood coagulation factor XIV, is a zymogen, that is, an inactive enzyme. The activated form plays an important role in regulating anticoagulation, inflammation, and cell death and maintaining the permeability of blood vessel walls in humans and other animals. Activated protein C (APC) performs these operations primarily by proteolytically inactivating proteins Factor Va and Factor VIIIa. APC is classified as a serine protease since it contains a residue of serine in its active site. In humans, protein C is encoded by the PROC gene, which is found on chromosome 2.

Coagulation factor X, or Stuart factor, is an enzyme of the coagulation cascade, encoded in humans by F10 gene. It is a serine endopeptidase. Factor X is synthesized in the liver and requires vitamin K for its synthesis.
Coagulation factor V, also less commonly known as proaccelerin or labile factor, is a protein involved in coagulation, encoded, in humans, by F5 gene. In contrast to most other coagulation factors, it is not enzymatically active but functions as a cofactor. Factor V deficiency leads to predisposition for hemorrhage, while some mutations predispose for thrombosis.

Factor XI, or plasma thromboplastin antecedent, is the zymogen form of factor XIa, one of the enzymes involved in coagulation. Like many other coagulation factors, it is a serine protease. In humans, factor XI is encoded by F11 gene.
The prothrombinase enzyme complex consists of factor Xa (a serine protease) and factor Va (a protein cofactor). The complex assembles on negatively charged phospholipid membranes in the presence of calcium ions. The prothrombinase complex catalyzes the conversion of prothrombin (factor II), an inactive zymogen, to thrombin (factor IIa), an active serine protease. The activation of thrombin is a critical reaction in the coagulation cascade, which functions to regulate hemostasis in the body. To produce thrombin, the prothrombinase complex cleaves two peptide bonds in prothrombin, one after Arg271 and the other after Arg320. Although it has been shown that factor Xa can activate prothrombin when unassociated with the prothrombinase complex, the rate of thrombin formation is severely decreased under such circumstances. The prothrombinase complex can catalyze the activation of prothrombin at a rate 3 x 105-fold faster than can factor Xa alone. Thus, the prothrombinase complex is required for the efficient production of activated thrombin and also for adequate hemostasis.
Prekallikrein (PK), also known as Fletcher factor, is an 85,000 Mr serine protease that complexes with high-molecular-weight kininogen. PK is the precursor of plasma kallikrein, which is a serine protease that activates kinins. PK is cleaved to produce kallikrein by activated Factor XII.
Kininogens are precursor proteins for kinins, biologically active polypeptides involved in blood coagulation, vasodilation, smooth muscle contraction, inflammatory regulation, and the regulation of the cardiovascular and renal systems.

Platelet factor 4 (PF4) is a small cytokine belonging to the CXC chemokine family that is also known as chemokine ligand 4 (CXCL4). This chemokine is released from alpha-granules of activated platelets during platelet aggregation, and promotes blood coagulation by moderating the effects of heparin-like molecules. Due to these roles, it is predicted to play a role in wound repair and inflammation. It is usually found in a complex with proteoglycan.

Coagulation factor XIII A chain, (FXIIIa) is a protein that in humans is encoded by the F13A1 gene.

Coagulation factor XIII B chain is a protein that in humans is encoded by the F13B gene.

Oscar Davis Ratnoff was an American physician who conducted research on the process of coagulation and blood-related disorders. Ratnoff discovered the substance later known as Factor XII and was one of the primary contributors to the delineation of the exact sequence that makes up the clotting cascade. He also made notable research contributions to the understanding of the complement system and to the detection and treatment of hemophilia.
Factor XII deficiency is a deficiency in the production of factor XII (FXII), a plasma glycoprotein and clotting factor that participates in the coagulation cascade and activates factor XI. FXII appears to be not essential for blood clotting, as individuals with this condition are usually asymptomatic and form blood clots in vivo. FXII deficiency tends to be identified during presurgical laboratory screening for bleeding disorders.

In the contact activation system or CAS, three proteins in the blood, factor XII (FXII), prekallikrein (PK) and high molecular weight kininogen (HK), bind to a surface and cause blood coagulation and inflammation. FXII and PK are proteases and HK is a non-enzymatic co-factor. The CAS can activate the kinin–kallikrein system and blood coagulation through its ability to activate multiple downstream proteins. The CAS is initiated when FXII binds to a surface and reciprocal activation of FXII and PK occurs, forming FXIIa and PKa. FXIIa can initiate the coagulation cascade by cleaving and activating factor XI (FXI), which leads to formation of a blood clot. Additionally, the CAS can activate the kinin–kallikrein system when PKa cleaves HK to form cHK, releasing a peptide known as bradykinin (BK). BK and its derivatives bind to bradykinin receptors B1 and B2 to mediate inflammation.