Hemolytic–uremic syndrome (HUS) is a group of blood disorders characterized by low red blood cells, acute kidney injury, and low platelets. Initial symptoms typically include bloody diarrhea, fever, vomiting, and weakness. Kidney problems and low platelets then occur as the diarrhea progresses. Children are more commonly affected, but most children recover without permanent damage to their health, although some children may have serious and sometimes life-threatening complications. Adults, especially the elderly, may present a more complicated presentation. Complications may include neurological problems and heart failure.

The complement system, also known as complement cascade, is a part of the immune system that enhances (complements) the ability of antibodies and phagocytic cells to clear microbes and damaged cells from an organism, promote inflammation, and attack the pathogen's cell membrane. It is part of the innate immune system, which is not adaptable and does not change during an individual's lifetime. The complement system can, however, be recruited and brought into action by antibodies generated by the adaptive immune system.

The alternative pathway is a type of cascade reaction of the complement system and is a component of the innate immune system, a natural defense against infections.

C3 convertase belongs to family of serine proteases and is necessary in innate immunity as a part of the complement system which eventuate in opsonisation of particles, release of inflammatory peptides, C5 convertase formation and cell lysis.

Complement receptor type 1 (CR1) also known as C3b/C4b receptor or CD35 is a protein that in humans is encoded by the CR1 gene.

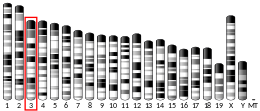
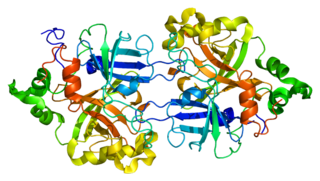
Complement component 3, often simply called C3, is a protein of the immune system that is found primarily in the blood. It plays a central role in the complement system of vertebrate animals and contributes to innate immunity. In humans it is encoded on chromosome 19 by a gene called C3.

C5 convertase is an enzyme belonging to a family of serine proteases that play key role in the innate immunity. It participates in the complement system ending with cell death.

Thrombomodulin (TM), CD141 or BDCA-3 is an integral membrane protein expressed on the surface of endothelial cells and serves as a cofactor for thrombin. It reduces blood coagulation by converting thrombin to an anticoagulant enzyme from a procoagulant enzyme. Thrombomodulin is also expressed on human mesothelial cell, monocyte and a dendritic cell subset.

Mannan-binding lectin serine protease 1 also known as mannose-associated serine protease 1 (MASP-1) is an enzyme that in humans is encoded by the MASP1 gene.

Factor D is a protein which in humans is encoded by the CFD gene. Factor D is involved in the alternative complement pathway of the complement system where it cleaves factor B.
Complement factor B is a protein that in humans is encoded by the CFB gene.
Complement control protein are proteins that interact with components of the complement system.

Factor H (FH) is a member of the regulators of complement activation family and is a complement control protein. It is a large, soluble glycoprotein that circulates in human plasma. Its principal function is to regulate the alternative pathway of the complement system, ensuring that the complement system is directed towards pathogens or other dangerous material and does not damage host tissue. Factor H regulates complement activation on self cells and surfaces by possessing both cofactor activity for the Factor I mediated C3b cleavage, and decay accelerating activity against the alternative pathway C3-convertase, C3bBb. Factor H exerts its protective action on self cells and self surfaces but not on the surfaces of bacteria or viruses. There are however, important exceptions, such as for example the bacterial pathogen, Neisseria meningitidis. This human pathogen has evolved mechanisms to recruit human FH and down-regulate the alternative pathway. Binding of FH permits the bacteria to proliferate in the bloodstream and cause disease.

CD46 complement regulatory protein also known as CD46 and Membrane Cofactor Protein is a protein which in humans is encoded by the CD46 gene. CD46 is an inhibitory complement receptor.

C3b is the larger of two elements formed by the cleavage of complement component 3, and is considered an important part of the innate immune system. C3b is potent in opsonization: tagging pathogens, immune complexes (antigen-antibody), and apoptotic cells for phagocytosis. Additionally, C3b plays a role in forming a C3 convertase when bound to Factor B, or a C5 convertase when bound to C4b and C2b or when an additional C3b molecule binds to the C3bBb complex.

Complement factor H-related protein 1 is a protein that in humans is encoded by the CFHR1 gene.

Complement factor H-related protein 3 is a protein that in humans is encoded by the CFHR3 gene.

Complement factor H-related protein 4 is a protein that in humans is encoded by the CFHR4 gene.

Complement component 4B (Chido blood group) is a kind of the Complement component 4 protein that in humans is encoded by the C4B gene.
Atypical hemolytic uremic syndrome (aHUS), also known as complement-mediated hemolytic uremic syndrome, is an extremely rare, life-threatening, progressive disease that frequently has a genetic component. In most cases it can be effectively controlled by interruption of the complement cascade. Particular monoclonal antibodies, discussed later in the article, have proven efficacy in many cases.