Tuberculosis (TB), also known colloquially as the "white death", or historically as consumption, is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, in which case it is known as latent tuberculosis. Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected. Typical symptoms of active TB are chronic cough with blood-containing mucus, fever, night sweats, and weight loss. Infection of other organs can cause a wide range of symptoms.

The Mantoux test or Mendel–Mantoux test is a tool for screening for tuberculosis (TB) and for tuberculosis diagnosis. It is one of the major tuberculin skin tests used around the world, largely replacing multiple-puncture tests such as the tine test. The Heaf test, a form of tine test, was used until 2005 in the UK, when it was replaced by the Mantoux test. The Mantoux test is endorsed by the American Thoracic Society and Centers for Disease Control and Prevention. It was also used in the USSR and is now prevalent in most of the post-Soviet states, although Soviet mantoux produced many false positives due to children's allergic reaction.
Radiology (X-rays) is used in the diagnosis of tuberculosis. Abnormalities on chest radiographs may be suggestive of, but are never diagnostic of TB, but can be used to rule out pulmonary TB.
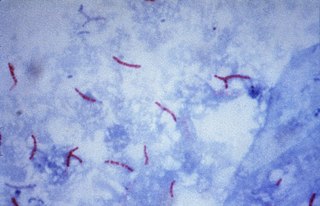
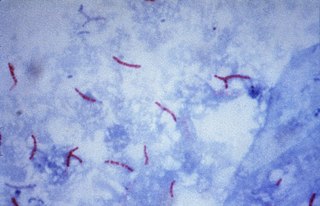
The Ziehl-Neelsen stain, also known as the acid-fast stain, is a bacteriological staining technique used in cytopathology and microbiology to identify acid-fast bacteria under microscopy, particularly members of the Mycobacterium genus. This staining method was initially introduced by Paul Ehrlich (1854–1915) and subsequently modified by the German bacteriologists Franz Ziehl (1859–1926) and Friedrich Neelsen (1854–1898) during the late 19th century.

Tuberculosis management describes the techniques and procedures utilized for treating tuberculosis (TB) or simply a treatment plan for TB.
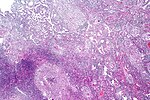
Peripheral tuberculous lymphadenitis is a form of tuberculosis infection occurring outside of the lungs. In general, it describes tuberculosis infection of the lymph nodes, leading to lymphadenopathy. When cervical lymph nodes are affected, it is commonly referred to as "Scrofula." A majority of tuberculosis infections affect the lungs, and extra-pulmonary tuberculosis infections account for the remainder; these most commonly involve the lymphatic system. Although the cervical region is most commonly affected, tuberculous lymphadenitis can occur all around the body, including the axillary and inguinal regions.

Miliary tuberculosis is a form of tuberculosis that is characterized by a wide dissemination into the human body and by the tiny size of the lesions (1–5 mm). Its name comes from a distinctive pattern seen on a chest radiograph of many tiny spots distributed throughout the lung fields with the appearance similar to millet seeds—thus the term "miliary" tuberculosis. Miliary TB may infect any number of organs, including the lungs, liver, and spleen. Miliary tuberculosis is present in about 2% of all reported cases of tuberculosis and accounts for up to 20% of all extra-pulmonary tuberculosis cases.

Mycobacterium avium-intracellulare infection (MAI) is an atypical mycobacterial infection, i.e. one with nontuberculous mycobacteria or NTM, caused by Mycobacterium avium complex (MAC), which is made of two Mycobacterium species, M. avium and M. intracellulare. This infection causes respiratory illness in birds, pigs, and humans, especially in immunocompromised people. In the later stages of AIDS, it can be very severe. It usually first presents as a persistent cough. It is typically treated with a series of three antibiotics for a period of at least six months.
Latent tuberculosis (LTB), also called latent tuberculosis infection (LTBI) is when a person is infected with Mycobacterium tuberculosis, but does not have active tuberculosis (TB). Active tuberculosis can be contagious while latent tuberculosis is not, and it is therefore not possible to get TB from someone with latent tuberculosis. The main risk is that approximately 10% of these people will go on to develop active tuberculosis. This is particularly true, and there is added risk, in particular situations such as medication that suppresses the immune system or advancing age.

Tuberculous meningitis, also known as TB meningitis or tubercular meningitis, is a specific type of bacterial meningitis caused by the Mycobacterium tuberculosis infection of the meninges—the system of membranes which envelop the central nervous system.
Lipoarabinomannan, also called LAM, is a glycolipid, and a virulence factor associated with Mycobacterium tuberculosis, the bacteria responsible for tuberculosis. Its primary function is to inactivate macrophages and scavenge oxidative radicals.
Interferon-γ release assays (IGRA) are medical tests used in the diagnosis of some infectious diseases, especially tuberculosis. Interferon-γ (IFN-γ) release assays rely on the fact that T-lymphocytes will release IFN-γ when exposed to specific antigens. These tests are mostly developed for the field of tuberculosis diagnosis, but in theory, may be used in the diagnosis of other diseases that rely on cell-mediated immunity, e.g. cytomegalovirus and leishmaniasis and COVID-19. For example, in patients with cutaneous adverse drug reactions, the challenge of peripheral blood lymphocytes with the drug causing the reaction produced a positive test result for half of the drugs tested.
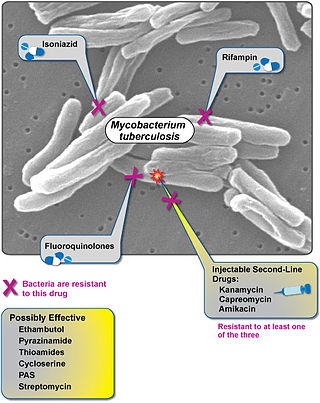
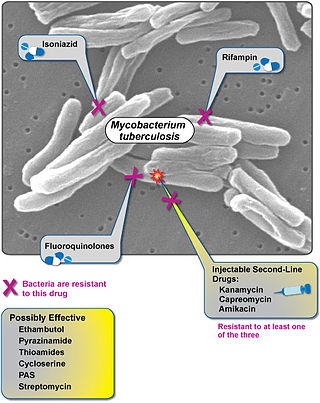
Extensively drug-resistant tuberculosis (XDR-TB) is a form of tuberculosis caused by bacteria that are resistant to some of the most effective anti-TB drugs. XDR-TB strains have arisen after the mismanagement of individuals with multidrug-resistant TB (MDR-TB).
The National Tuberculosis Elimination Programme (NTEP), earlier known as the Revised National Tuberculosis Control Programme (RNTCP), is the Public Health initiative of the Government of India that organizes its anti-Tuberculosis efforts. It functions as a flagship component of the National Health Mission (NHM) and provides technical and managerial leadership to anti-tuberculosis activities in the country. As per the National Strategic Plan 2017–25, the program has a vision of achieving a "TB free India",with a strategies under the broad themes of "Prevent, Detect,Treat and Build pillars for universal coverage and social protection". The program provides, various free of cost, quality tuberculosis diagnosis and treatment services across the country through the government health system.
Interferon-gamma release assays (IGRAs) are diagnostic tools for latent tuberculosis infection (LTBI). They are surrogate markers of Mycobacterium tuberculosis infection and indicate a cellular immune response to M. tuberculosis if the latter is present.
T-SPOT.TB is a type of ELISpot assay used for tuberculosis diagnosis, which belongs to the group of interferon gamma release assays. The test is manufactured by Oxford Immunotec in the UK. It is available in most European countries, the United States as well as various other countries. It was developed by researchers at the University of Oxford in England.
Tuberculous pericarditis is a form of pericarditis. It is a condition in which the pericardium surrounding the heart is infected by the bacterial species Mycobacterium tuberculosis. Tuberculous pericarditis accounts for a significant percentage of presentations of tuberculosis worldwide. The condition has four stages of disease which manifests with clinical presentations ranging from acute pericarditis to overt heart failure. Tuberculous pericarditis is an under-diagnosed condition. Diagnosis often requires a range of diagnostic tools, including pericardiocentesis, biochemical tests, and imaging. Treatment of this disease is similar to treatment of pulmonary tuberculosis. Alternative treatment options to reduce cardiac complications are also available.
The Xpert MTB/RIF is a cartridge-based nucleic acid amplification test (NAAT) for simultaneous rapid tuberculosis diagnosis and rapid antibiotic sensitivity test. It is an automated diagnostic test that can identify Mycobacterium tuberculosis (MTB) DNA and resistance to rifampicin (RIF). It was co-developed by the laboratory of Professor David Alland at the University of Medicine and Dentistry of New Jersey (UMDNJ), Cepheid Inc. and Foundation for Innovative New Diagnostics, with additional financial support from the US National Institutes of Health (NIH).

The National Tuberculosis Institute (NTIB) is a Government of India institute, under the Directorate General of Health Services, Ministry of Health and Family Welfare, dedicated to advanced research on Tuberculosis. The Institute is located along Bellary Road, in Bengaluru, Karnataka state, India.
Diagnostic delay is the time interval between the onset of symptoms and confirmed diagnosis of a disease. For a variety of reasons, including the mitigation of disease severity and financial expense, it is desirable for this delay to be minimized.