A human pathogen is a pathogen that causes disease in humans.

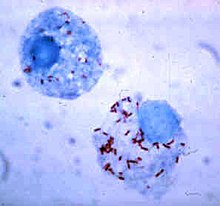
Rickettsia is a genus of nonmotile, gram-negative, nonspore-forming, highly pleomorphic bacteria that may occur in the forms of cocci, bacilli, or threads. The genus was named after Howard Taylor Ricketts in honor of his pioneering work on tick-borne spotted fever.

Rocky Mountain spotted fever (RMSF) is a bacterial disease spread by ticks. It typically begins with a fever and headache, which is followed a few days later with the development of a rash. The rash is generally made up of small spots of bleeding and starts on the wrists and ankles. Other symptoms may include muscle pains and vomiting. Long-term complications following recovery may include hearing loss or loss of part of an arm or leg.

Boutonneuse fever is a fever as a result of a rickettsial infection caused by the bacterium Rickettsia conorii and transmitted by the dog tick Rhipicephalus sanguineus. Boutonneuse fever can be seen in many places around the world, although it is endemic in countries surrounding the Mediterranean Sea. This disease was first described in Tunisia in 1910 by Conor and Bruch and was named boutonneuse due to its papular skin-rash characteristics.

Coxiella burnetii is an obligate intracellular bacterial pathogen, and is the causative agent of Q fever. The genus Coxiella is morphologically similar to Rickettsia, but with a variety of genetic and physiological differences. C. burnetii is a small Gram-negative, coccobacillary bacterium that is highly resistant to environmental stresses such as high temperature, osmotic pressure, and ultraviolet light. These characteristics are attributed to a small cell variant form of the organism that is part of a biphasic developmental cycle, including a more metabolically and replicatively active large cell variant form. It can survive standard disinfectants, and is resistant to many other environmental changes like those presented in the phagolysosome.
Tick-borne diseases, which afflict humans and other animals, are caused by infectious agents transmitted by tick bites. They are caused by infection with a variety of pathogens, including rickettsia and other types of bacteria, viruses, and protozoa. The economic impact of tick-borne diseases is considered to be substantial in humans, and tick-borne diseases are estimated to affect ~80 % of cattle worldwide. Most of these pathogens require passage through vertebrate hosts as part of their life cycle. Tick-borne infections in humans, farm animals, and companion animals are primarily associated with wildlife animal reservoirs. Many tick-borne infections in humans involve a complex cycle between wildlife animal reservoirs and tick vectors. The survival and transmission of these tick-borne viruses are closely linked to their interactions with tick vectors and host cells. These viruses are classified into different families, including Asfarviridae, Reoviridae, Rhabdoviridae, Orthomyxoviridae, Bunyaviridae, and Flaviviridae.

Meningoencephalitis, also known as herpes meningoencephalitis, is a medical condition that simultaneously resembles both meningitis, which is an infection or inflammation of the meninges, and encephalitis, which is an infection or inflammation of the brain tissue.
A rickettsiosis is a disease caused by intracellular bacteria.

Orientia tsutsugamushi is a mite-borne bacterium belonging to the family Rickettsiaceae and is responsible for a disease called scrub typhus in humans. It is a natural and an obligate intracellular parasite of mites belonging to the family Trombiculidae. With a genome of only 2.0–2.7 Mb, it has the most repeated DNA sequences among bacterial genomes sequenced so far. The disease, scrub typhus, occurs when infected mite larvae accidentally bite humans. This infection can prove fatal if prompt doxycycline therapy is not started.

Pathogenic bacteria are bacteria that can cause disease. This article focuses on the bacteria that are pathogenic to humans. Most species of bacteria are harmless and are often beneficial but others can cause infectious diseases. The number of these pathogenic species in humans is estimated to be fewer than a hundred. By contrast, several thousand species are part of the gut flora present in the digestive tract.

Rhipicephalus sanguineus, commonly called the brown dog tick, kennel tick, or pantropical dog tick, is a species of tick found worldwide, but more commonly in warmer climates. This species is unusual among ticks in that its entire lifecycle can be completed indoors. The brown dog tick is easily recognized by its reddish-brown color, elongated body shape, and hexagonal basis capituli. Adults are 2.28 to 3.18 mm in length and 1.11 to 1.68 mm in width. They do not have ornamentation on their backs.
Rickettsia typhi is a small, aerobic, obligate intracellular, rod shaped gram negative bacterium. It belongs to the typhus group of the Rickettsia genus, along with R. prowazekii. R. typhi has an uncertain history, as it may have long gone shadowed by epidemic typhus. This bacterium is recognized as a biocontainment level 2/3 organism. R. typhi is a flea-borne disease that is best known to be the causative agent for the disease murine typhus, which is an endemic typhus in humans that is distributed worldwide. As with all rickettsial organisms, R. typhi is a zoonotic agent that causes the disease murine typhus, displaying non-specific mild symptoms of fevers, headaches, pains and rashes. There are two cycles of R. typhi transmission from animal reservoirs containing R. typhi to humans: a classic rat-flea-rat cycle that is most well studied and common, and a secondary periodomestic cycle that could involve cats, dogs, opossums, sheep, and their fleas.

African tick bite fever (ATBF) is a bacterial infection spread by the bite of a tick. Symptoms may include fever, headache, muscle pain, and a rash. At the site of the bite there is typically a red skin sore with a dark center. The onset of symptoms usually occurs 4–10 days after the bite. Complications are rare but may include joint inflammation. Some people do not develop symptoms.
Queensland tick typhus is a zoonotic disease caused by the bacterium Rickettsia australis. It is transmitted by the ticks Ixodes holocyclus and Ixodes tasmani.
Rickettsia australis is a bacterium that causes a medical condition called Queensland tick typhus. The probable vectors are the tick species, Ixodes holocyclus and Ixodes tasmani. Small marsupials are suspected reservoirs of this bacterium.

Rickettsia parkeri is a gram-negative intracellular bacterium. The organism is found in the Western Hemisphere and is transmitted via the bite of hard ticks of the genus Amblyomma. R. parkeri causes mild spotted fever disease in humans, whose most common signs and symptoms are fever, an eschar at the site of tick attachment, rash, headache, and muscle aches. Doxycycline is the most common drug used to reduce the symptoms associated with disease.
Rickettsia felis is a species of bacterium, the pathogen that causes cat-flea typhus in humans, also known as flea-borne spotted fever. Rickettsia felis also is regarded as the causative organism of many cases of illnesses generally classed as fevers of unknown origin in humans in Africa.
In biology, a pathogen, in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ.
Rickettsia peacockii is a species of gram negative Alphaproteobacteria of the spotted fever group, identified from Rocky Mountain wood ticks. Its type strain is SkalkahoT. The organism is passed transstadially and transovarially, and infections are localized in ovarial tissues.

Haemaphysalis leporispalustris, the rabbit tick, is a species of tick that is widely distributed in the Americas, stretching from Alaska to Argentina. H. leporispalustris is known to have one of the largest distributions for a tick originating in the New World. It is a three-host tick and a member of the family Ixodidae, commonly called the "hard ticks," and the genus Haemaphysalis. Its common hosts are rabbits, hares, and sometimes ground-feeding birds. H. leporispalustris has a rigid scutum and a prominent capitulum projecting forward from its body and is often said to look like the "wood tick". It has a hemimetabolic life cycle. H. leporispalustris does not play a prominent role in disease transmission in humans but is a vector for disease in other animals.