Brain abscess is an abscess within the brain tissue caused by inflammation and collection of infected material coming from local or remote infectious sources. The infection may also be introduced through a skull fracture following a head trauma or surgical procedures. Brain abscess is usually associated with congenital heart disease in young children. It may occur at any age but is most frequent in the third decade of life.

The danger triangle of the face consists of the area from the corners of the mouth to the bridge of the nose, including the nose and maxilla. Due to the special nature of the blood supply to the human nose and surrounding area, it is possible, albeit extremely unlikely, for retrograde infection from the nasal area to spread to the brain, causing cavernous sinus thrombosis, meningitis, or brain abscess.

Fusobacterium is a genus of obligate anaerobic, Gram-negative, non-sporeforming bacteria belonging to Gracilicutes. Individual cells are slender, rod-shaped bacilli with pointed ends. Fusobacterium was discovered in 1900 by Courmont and Cade and is common in the flora of humans.

Pharyngitis is inflammation of the back of the throat, known as the pharynx. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, difficulty swallowing, swollen lymph nodes, and a hoarse voice. Symptoms usually last 3–5 days, but can be longer depending on cause. Complications can include sinusitis and acute otitis media. Pharyngitis is a type of upper respiratory tract infection.
Bloodstream infections (BSIs), septicemia which include bacteremias when the infections are bacterial and fungemias when the infections are fungal, are infections present in the blood. Blood is normally a sterile environment, so the detection of microbes in the blood is always abnormal. A bloodstream infection is different from sepsis, which is the host response to bacteria.

Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines septic shock as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by requiring a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater and having serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%.

Cellulitis is usually a bacterial infection involving the inner layers of the skin. It specifically affects the dermis and subcutaneous fat. Signs and symptoms include an area of redness which increases in size over a few days. The borders of the area of redness are generally not sharp and the skin may be swollen. While the redness often turns white when pressure is applied, this is not always the case. The area of infection is usually painful. Lymphatic vessels may occasionally be involved, and the person may have a fever and feel tired.

Tonsillitis is inflammation of the tonsils in the upper part of the throat. It can be acute or chronic. Acute tonsillitis typically has a rapid onset. Symptoms may include sore throat, fever, enlargement of the tonsils, trouble swallowing, and enlarged lymph nodes around the neck. Complications include peritonsillar abscess (Quinsy).

Peritonsillar abscess (PTA), also known as quinsy, is an accumulation of pus due to an infection behind the tonsil. Symptoms include fever, throat pain, trouble opening the mouth, and a change to the voice. Pain is usually worse on one side. Complications may include blockage of the airway or aspiration pneumonitis.

Mastoiditis is the result of an infection that extends to the air cells of the skull behind the ear. Specifically, it is an inflammation of the mucosal lining of the mastoid antrum and mastoid air cell system inside the mastoid process. The mastoid process is the portion of the temporal bone of the skull that is behind the ear. The mastoid process contains open, air-containing spaces. Mastoiditis is usually caused by untreated acute otitis media and used to be a leading cause of child mortality. With the development of antibiotics, however, mastoiditis has become quite rare in developed countries where surgical treatment is now much less frequent and more conservative, unlike former times.

Lung abscess is a type of liquefactive necrosis of the lung tissue and formation of cavities containing necrotic debris or fluid caused by microbial infection.

Lymphangitis is an inflammation or an infection of the lymphatic channels that occurs as a result of infection at a site distal to the channel. The most common cause of lymphangitis in humans is Streptococcus pyogenes, hemolytic streptococci, and in some cases, mononucleosis, cytomegalovirus, tuberculosis, syphilis, and the fungus Sporothrix schenckii. Lymphangitis is sometimes mistakenly called "blood poisoning". In reality, "blood poisoning" is synonymous with sepsis.
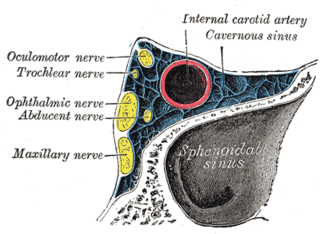
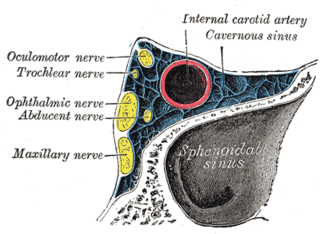
Cavernous sinus thrombosis (CST) is the formation of a blood clot within the cavernous sinus, a cavity at the base of the brain which drains deoxygenated blood from the brain back to the heart. This is a rare disorder and can be of two types–septic cavernous thrombosis and aseptic cavernous thrombosis. The most common form is septic cavernous sinus thrombosis. The cause is usually from a spreading infection in the nose, sinuses, ears, or teeth. Staphylococcus aureus and Streptococcus are often the associated bacteria.
Fusobacterium necrophorum is a species of bacteria responsible for Lemierre's syndrome. It has also been known to cause sinusitis, mastoiditis, and odontogenic infections.
A septic embolism is a type of embolism that is infected with bacteria, resulting in the formation of pus. These may become dangerous if dislodged from their original location. Like other emboli, a septic embolism may be fatal.
Septic abortion describes any type of abortion, due to an upper genital tract bacterial infection including the inflammation of the endometrium during or after 20 weeks of gestation. The genital tract during this period is particularly vulnerable to infection, and sepsis in most cases is caused by a combination of factors both due to facility conditions and/or individual predispositions. The infection often starts in the placenta and fetus, with a potential complication of also affecting the uterus, that can result in sepsis spreading to surrounding organs, or pelvic infections.
Anaerobic infections are caused by anaerobic bacteria. Obligately anaerobic bacteria do not grow on solid media in room air ; facultatively anaerobic bacteria can grow in the presence or absence of air. Microaerophilic bacteria do not grow at all aerobically or grow poorly, but grow better under 10% carbon dioxide or anaerobically. Anaerobic bacteria can be divided into strict anaerobes that can not grow in the presence of more than 0.5% oxygen and moderate anaerobic bacteria that are able of growing between 2 and 8% oxygen. Anaerobic bacteria usually do not possess catalase, but some can generate superoxide dismutase which protects them from oxygen.
Septic pelvic thrombophlebitis (SPT), also known as suppurative pelvic thrombophlebitis, is a rare postpartum complication which consists of a persistent postpartum fever that is not responsive to broad-spectrum antibiotics, in which pelvic infection leads to infection of the vein wall and intimal damage leading to thrombogenesis in the ovarian veins. The thrombus is then invaded by microorganisms. Ascending infections cause 99% of postpartum SPT.

Superficial vein thrombosis (SVT) is a blood clot formed in a superficial vein, a vein near the surface of the body. Usually there is thrombophlebitis, which is an inflammatory reaction around a thrombosed vein, presenting as a painful induration with redness. SVT itself has limited significance when compared to a deep vein thrombosis (DVT), which occurs deeper in the body at the deep venous system level. However, SVT can lead to serious complications, and is therefore no longer regarded as a benign condition. If the blood clot is too near the saphenofemoral junction there is a higher risk of pulmonary embolism, a potentially life-threatening complication.

A lung cavity or pulmonary cavity is an abnormal, thick-walled, air-filled space within the lung. Cavities in the lung can be caused by infections, cancer, autoimmune conditions, trauma, congenital defects, or pulmonary embolism. The most common cause of a single lung cavity is lung cancer. Bacterial, mycobacterial, and fungal infections are common causes of lung cavities. Globally, tuberculosis is likely the most common infectious cause of lung cavities. Less commonly, parasitic infections can cause cavities. Viral infections almost never cause cavities. The terms cavity and cyst are frequently used interchangeably; however, a cavity is thick walled, while a cyst is thin walled. The distinction is important because cystic lesions are unlikely to be cancer, while cavitary lesions are often caused by cancer.