Eosinophils, sometimes called eosinophiles or, less commonly, acidophils, are a variety of white blood cells and one of the immune system components responsible for combating multicellular parasites and certain infections in vertebrates. Along with mast cells and basophils, they also control mechanisms associated with allergy and asthma. They are granulocytes that develop during hematopoiesis in the bone marrow before migrating into blood, after which they are terminally differentiated and do not multiply. They form about 2 to 3% of white blood cells in the body.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.

Infliximab, a chimeric monoclonal antibody, sold under the brand name Remicade among others, is a medication used to treat a number of autoimmune diseases. This includes Crohn's disease, ulcerative colitis, rheumatoid arthritis, ankylosing spondylitis, psoriasis, psoriatic arthritis, and Behçet's disease. It is given by slow injection into a vein, typically at six- to eight-week intervals.
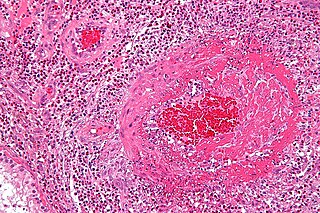
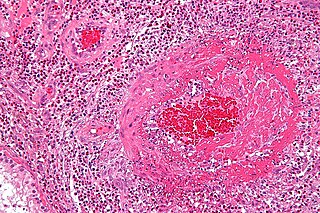
Eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels (vasculitis) in persons with a history of airway allergic hypersensitivity (atopy).
Ustekinumab, sold under the brand name Stelara among others, is a monoclonal antibody medication developed by Janssen Pharmaceuticals, for the treatment of Crohn's disease, ulcerative colitis, plaque psoriasis and psoriatic arthritis, targeting both IL-12 and IL-23.
Mepolizumab, sold under the brand name Nucala by GlaxoSmithKline, is a humanized monoclonal antibody used for the treatment of severe eosinophilic asthma, eosinophilic granulomatosis, and hypereosinophilic syndrome (HES). It recognizes and blocks interleukin-5 (IL-5), a signalling protein of the immune system.
Lebrikizumab is a humanized monoclonal antibody and an investigational immunosuppressive medication for the treatment of asthma that cannot be adequately controlled with inhalable glucocorticoids. It was created by Tanox under the name TNX-650, and a phase I clinical trial for refractory Hodgkin’s lymphoma had been performed when Genentech acquired Tanox in 2007. It has successfully completed a Phase II clinical trial for the treatment of asthma.
Benralizumab, sold under the brand name Fasenra, is a monoclonal antibody directed against the alpha chain of the interleukin-5 receptor (CD125). It was developed by MedImmune for the treatment of asthma.
Ixekizumab, sold under the brand name Taltz, is an injectable medication for the treatment of autoimmune diseases. Chemically, it is a form of a humanized monoclonal antibody. The substance acts by binding interleukin 17A and neutralizing it, reducing inflammation.

Secukinumab, sold under the brand name Cosentyx among others, is a human IgG1κ monoclonal antibody used for the treatment of psoriasis, ankylosing spondylitis, and psoriatic arthritis. It binds to the protein interleukin (IL)-17A and is marketed by Novartis.
Dupilumab, sold under the brand name Dupixent, is a monoclonal antibody blocking interleukin 4 and interleukin 13, used for allergic diseases such as eczema, asthma and nasal polyps which result in chronic sinusitis. It is also used for the treatment of eosinophilic esophagitis and prurigo nodularis.
Tildrakizumab, sold under the brand names Ilumya and Ilumetri, is a monoclonal antibody designed for the treatment of immunologically mediated inflammatory disorders. It is approved for the treatment of adult patients with moderate-to-severe plaque psoriasis in the United States and the European Union.
Guselkumab, sold under the brand name Tremfya, is a monoclonal antibody against interleukin-23 used for the treatment of plaque psoriasis.

Pembrolizumab, sold under the brand name Keytruda, is a humanized antibody used in cancer immunotherapy that treats melanoma, lung cancer, head and neck cancer, Hodgkin lymphoma, stomach cancer, cervical cancer, and certain types of breast cancer. It is given by slow injection into a vein.
Dinutuximab and dinutuximab beta are monoclonal antibodies used as a second-line treatment for children with high-risk neuroblastoma. Each antibody is made of both mouse and human components and targets glycolipid GD2, expressed on neuroblastoma cells and on normal cells of neuroectodermal origin, including the central nervous system and peripheral nerves. They differ in that dinutuximab is manufactured using mouse cells, and dinutuximab beta is manufactured using hamster cells. The dosing regime differs, and dinutuximab is given in combination with granulocyte-macrophage colony stimulating factor (GM-CSF), interleukin-2 (IL-2) and 13-cis-retinoic acid (RA), while dinutuximab beta can be given alone.

Tezepelumab, sold under the brand name Tezspire, is a human monoclonal antibody used for the treatment of asthma. Tezepelumab blocks thymic stromal lymphopoietin (TSLP), an epithelial cytokine that has been suggested to be critical in the initiation and persistence of airway inflammation.
Lanadelumab, sold under the brand name Takhzyro, is a human monoclonal antibody that targets plasma kallikrein (pKal) in order to promote prevention of angioedema in people with hereditary angioedema. Lanadelumab, was approved in the United States as the first monoclonal antibody indicated for prophylactic treatment to prevent hereditary angioedema attacks. Lanadelumab is the first treatment for hereditary angioedema prevention made by using cells within a lab, not human plasma.
Lirentelimab is a humanized nonfucosylated monoclonal antibody that targets sialic acid-binding Ig-like lectin 8 (SIGLEC8). In a randomized clinical trial, lirentelimab was found to improve eosinophil counts and symptoms in individuals with eosinophilic gastritis and duodenitis. Adverse reactions include infusion reactions, which are mild to moderate and typically occur following the first infusion.
Bamlanivimab/etesevimab is a combination of two monoclonal antibodies, bamlanivimab and etesevimab, administered together via intravenous infusion as a treatment for COVID-19. Both types of antibody target the surface spike protein of SARS‑CoV‑2.