Athlete's foot, known medically as tinea pedis, is a common skin infection of the feet caused by a fungus. Signs and symptoms often include itching, scaling, cracking and redness. In rare cases the skin may blister. Athlete's foot fungus may infect any part of the foot, but most often grows between the toes. The next most common area is the bottom of the foot. The same fungus may also affect the nails or the hands. It is a member of the group of diseases known as tinea.

Tinea capitis is a cutaneous fungal infection (dermatophytosis) of the scalp. The disease is primarily caused by dermatophytes in the genera Trichophyton and Microsporum that invade the hair shaft. The clinical presentation is typically single or multiple patches of hair loss, sometimes with a 'black dot' pattern, that may be accompanied by inflammation, scaling, pustules, and itching. Uncommon in adults, tinea capitis is predominantly seen in pre-pubertal children, more often boys than girls.

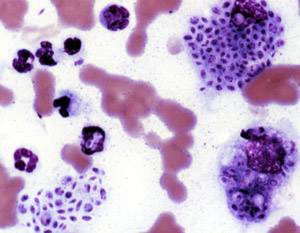
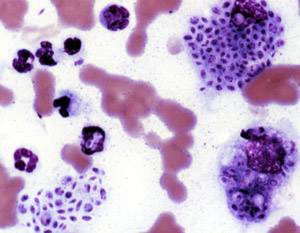
Zygomycosis is the broadest term to refer to infections caused by bread mold fungi of the zygomycota phylum. However, because zygomycota has been identified as polyphyletic, and is not included in modern fungal classification systems, the diseases that zygomycosis can refer to are better called by their specific names: mucormycosis, phycomycosis and basidiobolomycosis. These rare yet serious and potentially life-threatening fungal infections usually affect the face or oropharyngeal cavity. Zygomycosis type infections are most often caused by common fungi found in soil and decaying vegetation. While most individuals are exposed to the fungi on a regular basis, those with immune disorders (immunocompromised) are more prone to fungal infection. These types of infections are also common after natural disasters, such as tornadoes or earthquakes, where people have open wounds that have become filled with soil or vegetative matter.

Fungal infection, also known as mycosis, is a disease caused by fungi. Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic. Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor. Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin. Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis. Signs and symptoms range widely. There is usually a rash with superficial infection. Fungal infection within the skin or under the skin may present with a lump and skin changes. Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.

Eumycetoma, also known as Madura foot, is a persistent fungal infection of the skin and the tissues just under the skin, affecting most commonly the feet, although it can occur in hands and other body parts. It starts as a painless wet nodule, which may be present for years before ulceration, swelling, grainy discharge and weeping from sinuses and fistulae, followed by bone deformity.

Dermatophytosis, also known as tinea and ringworm, is a fungal infection of the skin, that may affect skin, hair, and nails. Typically it results in a red, itchy, scaly, circular rash. Hair loss may occur in the area affected. Symptoms begin four to fourteen days after exposure. The types of dermatophytosis are typically named for area of the body that they affect. Multiple areas can be affected at a given time.

Onychomycosis, also known as tinea unguium, is a fungal infection of the nail. Symptoms may include white or yellow nail discoloration, thickening of the nail, and separation of the nail from the nail bed. Fingernails may be affected, but it is more common for toenails. Complications may include cellulitis of the lower leg. A number of different types of fungus can cause onychomycosis, including dermatophytes and Fusarium. Risk factors include athlete's foot, other nail diseases, exposure to someone with the condition, peripheral vascular disease, and poor immune function. The diagnosis is generally suspected based on the appearance and confirmed by laboratory testing.

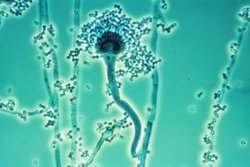
An aspergilloma is a clump of mold which exists in a body cavity such as a paranasal sinus or an organ such as the lung. By definition, it is caused by fungi of the genus Aspergillus.
Sporotrichosis, also known as rose handler's disease, is a fungal infection that may be localised to skin, lungs, bone and joint, or become systemic. It presents with firm painless nodules that later ulcerate. Following initial exposure to Sporothrix schenckii, the disease typically progresses over a period of a week to several months. Serious complications may develop in people who have a weakened immune system.
Phycomycosis is an uncommon condition of the gastrointestinal tract and skin most commonly found in dogs and horses. The condition is caused by a variety of molds and fungi, and individual forms include pythiosis, zygomycosis, and lagenidiosis. Pythiosis is the most common type and is caused by Pythium, a type of water mould. Zygomycosis can also be caused by two types of zygomycetes, Entomophthorales and Mucorales. The latter type of zygomycosis is also referred to as mucormycosis. Lagenidiosis is caused by a Lagenidium species, which like Pythium is a water mould. Since both pythiosis and lagenidiosis are caused by organisms from the Oomycetes and not the kingdom fungi, they are sometimes collectively referred to as oomycosis.
Talaromycosis is a fungal infection that presents with painless skin lesions of the face and neck, as well as an associated fever, anaemia, and enlargement of the lymph glands and liver.

Aspergillosis is a fungal infection of usually the lungs, caused by the genus Aspergillus, a common mould that is breathed in frequently from the air, but does not usually affect most people. It generally occurs in people with lung diseases such as asthma, cystic fibrosis or tuberculosis, or COVID-19 or those who are immunocompromized such as those who have had a stem cell or organ transplant or those who take medications such as steroids and some cancer treatments which suppress the immune system. Rarely, it can affect skin.

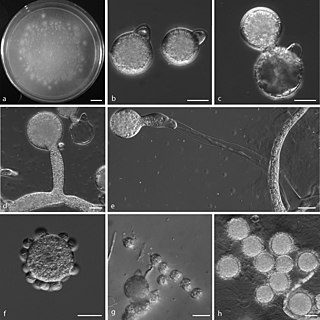
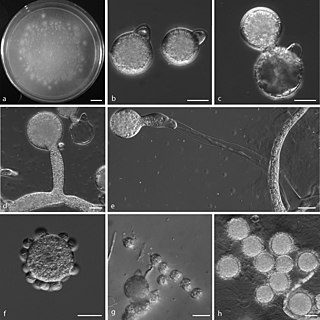
Basidiobolus ranarum is a filamentous fungus with worldwide distribution. The fungus was first isolated by Eidam in 1886. It can saprophytically live in the intestines of mainly cold-blooded vertebrates and on decaying fruits and soil. The fungus prefers glucose as a carbon source and grows rapidly at room temperature. Basidiobolus ranarum is also known as a cause of subcutaneous zygomycosis, usually causing granulomatous infections on a host's limbs. Infections are generally geographically limited to tropical and subtropical regions such as East and West Africa. Subcutaneous zygomycosis caused by B. ranarum is a rare disease and predominantly affects children and males. Common subcutaneous zygomycosis shows characteristic features and is relatively easy to be diagnosed; while, certain rare cases might show non-specific clinical features that might pose a difficulty on its identification. Although disease caused by this fungus is known to resolve spontaneously on its own, there are a number of treatments available.

Tinea nigra, also known as superficial phaeohyphomycosis and Tinea nigra palmaris et plantaris, is a superficial fungal infection, a type of phaeohyphomycosis rather than a tinea, that causes usually a single 1–5 cm dark brown-black, non-scaly, flat, painless patch on the palms of the hands and the soles of the feet of healthy people. There may be multiple spots. The macules occasionally extend to the fingers, toes, and nails, and may be reported on the chest, neck, or genital area. Tinea nigra infections can present with multiple macules that can be mottled or velvety in appearance, and may be oval or irregular in shape. The macules can be anywhere from a few mm to several cm in size.
A sinus is a sac or cavity in any organ or tissue, or an abnormal cavity or passage. In common usage, "sinus" usually refers to the paranasal sinuses, which are air cavities in the cranial bones, especially those near the nose and connecting to it. Most individuals have four paired cavities located in the cranial bone or skull.

Mucormycosis, also known as black fungus, is a serious fungal infection that comes under fulminant fungal sinusitis, usually in people who are immunocompromised. It is curable only when diagnosed early. Symptoms depend on where in the body the infection occurs. It most commonly infects the nose, sinuses, eyes and brain resulting in a runny nose, one-sided facial swelling and pain, headache, fever, blurred vision, bulging or displacement of the eye (proptosis), and tissue death. Other forms of disease may infect the lungs, stomach and intestines, and skin. The fatality rate is about 54%.
Conidiobolus coronatus is a saprotrophic fungus, first described by Costantin in 1897 as Boudierella coronata. Though this fungus has also been known by the name Entomophthora coronata, the correct name is Conidiobolus coronatus. C. coronatus is able to infect humans and animals, and the first human infection with C. coronatus was reported in Jamaica in 1965.
Phaeohyphomycosis is a diverse group of fungal infections, caused by dematiaceous fungi whose morphologic characteristics in tissue include hyphae, yeast-like cells, or a combination of these. It can be associated with an array of melanistic filamentous fungi including Alternaria species, Exophiala jeanselmei, and Rhinocladiella mackenziei.
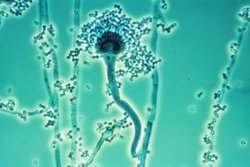
Fungal sinusitis or fungal rhinosinusitis is the inflammation of the lining mucosa of the paranasal sinuses due to a fungal infection. It occurs in people with reduced immunity. The maxillary sinus is the most commonly involved. Fungi responsible for fungal sinusitis are Aspergillus fumigatus (90%), Aspergillus flavus, and Aspergillus niger. Fungal sinusitis occurs most commonly in middle-aged populations. Diabetes mellitus is the most common risk factor involved.

Aspergillus felis is a heterothallic species of fungus in the genus Aspergillus which can cause aspergillosis in humans, dogs and cats. It was described for the first time in 2013 after being isolated from different hosts worldwide.