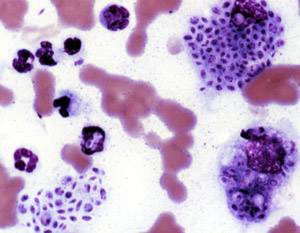
Coccidioidomycosis, commonly known as cocci, Valley fever, as well as California fever, desert rheumatism, or San Joaquin Valley fever, is a mammalian fungal disease caused by Coccidioides immitis or Coccidioides posadasii. Coccidioidomycosis is endemic in certain parts of the United States in Arizona, California, Nevada, New Mexico, Texas, Utah, and northern Mexico.

Histoplasmosis is a fungal infection caused by Histoplasma capsulatum. Symptoms of this infection vary greatly, but the disease affects primarily the lungs. Occasionally, other organs are affected; called disseminated histoplasmosis, it can be fatal if left untreated.

Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behavior. It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.

Coccidioides immitis is a pathogenic fungus that resides in the soil in certain parts of the southwestern United States, northern Mexico, and a few other areas in the Western Hemisphere.

Blastomycosis, also known as Gilchrist's disease, is a fungal infection, typically of the lungs, which can spread to brain, stomach, intestine and skin, where it appears as crusting purplish warty plaques with a roundish bumpy edge and central depression. Only about half of people with the disease have symptoms, which can include fever, cough, night sweats, muscle pains, weight loss, chest pain, and feeling tired. Symptoms usually develop between three weeks and three months after breathing in the spores. In 25% to 40% of cases, the infection also spreads to other parts of the body, such as the skin, bones or central nervous system. Although blastomycosis is especially dangerous for those with weak immune systems, most people diagnosed with blastomycosis have healthy immune systems.

Tinea capitis is a cutaneous fungal infection (dermatophytosis) of the scalp. The disease is primarily caused by dermatophytes in the genera Trichophyton and Microsporum that invade the hair shaft. The clinical presentation is typically single or multiple patches of hair loss, sometimes with a 'black dot' pattern, that may be accompanied by inflammation, scaling, pustules, and itching. Uncommon in adults, tinea capitis is predominantly seen in pre-pubertal children, more often boys than girls.

Chromoblastomycosis is a long-term fungal infection of the skin and subcutaneous tissue.

Dermatophytosis, also known as ringworm, is a fungal infection of the skin. Typically it results in a red, itchy, scaly, circular rash. Hair loss may occur in the area affected. Symptoms begin four to fourteen days after exposure. Multiple areas can be affected at a given time.

Onychomycosis, also known as tinea unguium, is a fungal infection of the nail. Symptoms may include white or yellow nail discoloration, thickening of the nail, and separation of the nail from the nail bed. Toenails or fingernails may be affected, but it is more common for toenails. Complications may include cellulitis of the lower leg. A number of different types of fungus can cause onychomycosis, including dermatophytes and Fusarium. Risk factors include athlete's foot, other nail diseases, exposure to someone with the condition, peripheral vascular disease, and poor immune function. The diagnosis is generally suspected based on the appearance and confirmed by laboratory testing.

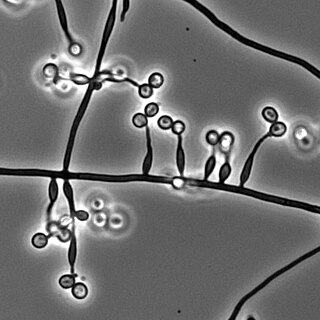
Pythiosis is a rare and deadly tropical disease caused by the oomycete Pythium insidiosum. Long regarded as being caused by a fungus, the causative agent was not discovered until 1987. It occurs most commonly in horses, dogs, and humans, with isolated cases in other large mammals. The disease is contracted after exposure to stagnant fresh water such as swamps, ponds, lakes, and rice paddies. P. insidiosum is different from other members of the genus in that human and horse hair, skin, and decaying animal and plant tissue are chemoattractants for its zoospores. Additionally, it is the only member in the genus known to infect mammals, while other members are pathogenic to plants and are responsible for some well-known plant diseases.
Talaromycosis is a fungal infection that presents with painless skin lesions of the face and neck, as well as an associated fever, anaemia, and enlargement of the lymph glands and liver.

Aspergillosis is a fungal infection of usually the lungs, caused by the genus Aspergillus, a common mould that is breathed in frequently from the air around, but does not usually affect most people. It generally occurs in people with lung diseases such as asthma, cystic fibrosis or tuberculosis, or those who have had a stem cell or organ transplant, and those who cannot fight infection because of medications they take such as steroids and some cancer treatments. Rarely, it can affect skin.

Paracoccidioidomycosis (PCM), also known as South American blastomycosis, is a fungal infection that can occur as a mouth and skin type, lymphangitic type, multi-organ involvement type (particularly lungs), or mixed type. If there are mouth ulcers or skin lesions, the disease is likely to be widespread. There may be no symptoms, or it may present with fever, sepsis, weight loss, large glands, or a large liver and spleen.

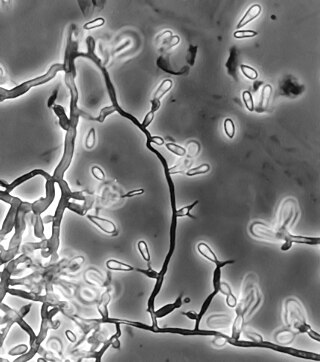
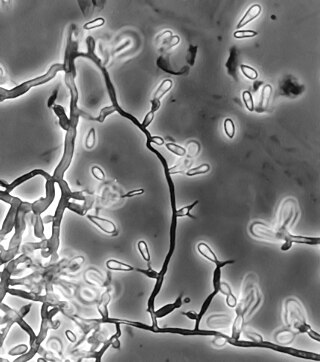
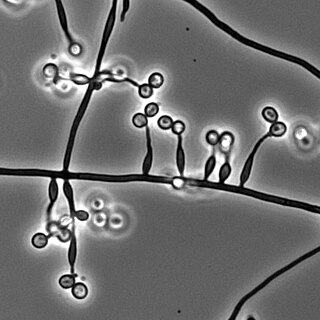
Sporothrix schenckii, a fungus that can be found worldwide in the environment, is named for medical student Benjamin Schenck, who in 1896 was the first to isolate it from a human specimen. The species is present in soil as well as in and on living and decomposing plant material such as peat moss. It can infect humans as well as animals and is the causative agent of sporotrichosis, commonly known as "rose handler's disease." The most common route of infection is the introduction of spores to the body through a cut or puncture wound in the skin. Infection commonly occurs in otherwise healthy individuals but is rarely life-threatening and can be treated with antifungals. In the environment it is found growing as filamentous hyphae. In host tissue it is found as a yeast. The transition between the hyphal and yeast forms is temperature dependent making S. schenckii a thermally dimorphic fungus.
Ochroconis gallopava, also called Dactylaria gallopava or Dactylaria constricta var. gallopava, is a member of genus Dactylaria. Ochroconis gallopava is a thermotolerant, darkly pigmented fungus that causes various infections in fowls, turkeys, poults, and immunocompromised humans first reported in 1986. Since then, the fungus has been increasingly reported as an agent of human disease especially in recipients of solid organ transplants. Ochroconis gallopava infection has a long onset and can involve a variety of body sites. Treatment of infection often involves a combination of antifungal drug therapy and surgical excision.

Phialophora verrucosa is a pathogenic, dematiaceous fungus that is a common cause of chromoblastomycosis. It has also been reported to cause subcutaneous phaeohyphomycosis and mycetoma in very rare cases. In the natural environment, it can be found in rotting wood, soil, wasp nests, and plant debris. P. verrucosa is sometimes referred to as Phialophora americana, a closely related environmental species which, along with P. verrucosa, is also categorized in the P. carrionii clade.
Edouard Drouhet was a physician, biologist, and medical mycologist who played a key role in understanding how anti-fungal agents such as ketoconazole and amphotericin-B can be used as therapeutic treatments in humans with superficial or deep-seated mycoses.
Metarhizium granulomatis is a fungus in the family Clavicipitaceae associated with systemic mycosis in veiled chameleons. The genus Metarhizium is known to infect arthropods, and collectively are referred to green-spored asexual pathogenic fungi. This species grows near the roots of plants and has been reported as an agent of disease in captive veiled chameleons. The etymology of the species epithet, "granulomatis" refers to the ability of the fungus to cause granulomatous disease in susceptible reptiles.
Arthrographis kalrae is an ascomycetous fungus responsible for human nail infections described in 1938 by Cochet as A. langeronii. A. kalrae is considered a weak pathogen of animals including human restricted to the outermost keratinized layers of tissue. Infections caused by this species are normally responsive to commonly used antifungal drugs with only very rare exceptions.
Sporothrix brasiliensis is a fungus that is commonly found in soil. It is an emerging fungal pathogen that is causing disease in humans and cats mainly in Brazil and other countries in South America.